Awareness about the necessity of vestibular rehabilitation education in Korean physical therapists
Article information
Abstract
Vestibular rehabilitation (VR) improves dizziness and vertigo, postural control, and quality of life. It is a beneficial and safe intervention for pa-tients with peripheral vestibular disease. Physical therapists play an im-portant role in treating them, but Korean physical therapists have little experience in VR or treating peripheral vestibular disease. Furthermore, there are few studies on the current status of Korean physical thera-pists regarding VR. Therefore, we aimed to identify the awareness and current status of Korean physical therapists regarding VR and to discuss the necessity of VR education. The data were obtained from an online survey conducted among 483 licensed physical therapists. In total, 393 questionnaires were analyzed, after excluding 90 questionnaires (18.6%) with poor answers. Most physical therapists had no VR education (75.6%) and had a high positive response for the necessity of VR education (68.2%) and intention to receive VR education (63.9%). There was a significant difference in clinical experience and intention to receive VR education (P<0.05) with respect to presence or absence of VR education. For the necessity of VR education, there was a statistically significant difference in academic background, institutional type, and intention to receive VR education (P<0.05). In conclusion, many physical therapists in Korea are very interested in VR education, and various factors have highlighted the need for VR education. Therefore, professional education for VR and the cooperation and attention of related medical staff are urgently required.
INTRODUCTION
Dizziness and vertigo are common and challenging complaints in a hospital. About 20%–30% of the world’s population has experienced dizziness and vertigo; in Korea, the prevalence rate is reported to be 16.70% in adults aged 40 and older (Koo et al., 2015; van Vugt et al., 2017; von Brevern and Neuhauser, 2011). The most common cause of dizziness and vertigo is peripheral vestibular disease including peripheral vestibular hypofunction, Meniere disease, and benign paroxysmal positional vertigo (van Vugt et al., 2017). To treat these diseases, various treatments such as vestibular rehabilitation (VR), medication, and canalith repositioning technique are applied. Of these, VR and medication are prescribed for patients with peripheral vestibular hypofunction (Fishman et al., 2011; Goudakos et al., 2014). Medication has limited effectiveness, and repeated treatment with the drug is known to interfere with vestibular function recovery. VR has been reported to have a positive effect (Kim, 2007; McDonnell and Hillier, 2015).
In the 1940s, otolaryngologist Cawthorne and physiotherapist Cooksey developed an exercise-based intervention to rehabilitate soldiers with brain damage and dizziness (Cawthorne, 1944; Cooksey, 1946). Since the 1970s, studies on physiology, pathology, functional tests, and compensatory mechanism of the vestibular system have been actively conducted, and rehabilitation therapy for patients with vestibular disorders has been administered since the 1980s (Courjon et al., 1977; Fetter and Zee, 1988; Igarashi et al., 1981; Lacour et al., 1985; Rhee et al., 2006). VR consists of eye, head, and body movements to promote recovery and compensation (van Vugt et al., 2017; Whitney et al., 2016). The goal of these exercises is to reduce dizziness and imbalance and improve quality of life (McDonnell and Hillier, 2015).
In Korea, VR was introduced in the 1990s; however, its implementation is infrequent because of the lack of understanding and cooperation among clinicians in rehabilitation medicine, psychiatry, and psychology (Rhee et al., 2006). Physical therapists also face difficulties in treating patients who have dizziness and vertigo because they are unaware of VR. Therefore, we aimed to identify the awareness and current status of Korean physical therapists regarding VR and to discuss the necessity of VR education.
MATERIALS AND METHODS
Participants and survey
This study conducted an online survey for 5 days from May 27 to May 31, 2019. Of the total of 483 questionnaires, 393 were analyzed, after excluding 90 (18.6%) with poor answers. Data collection was performed after explaining the purpose of this study and obtaining informed consent from the participants. The questionnaire consisted of six questions on general characteristics, five questions in the field of physical therapy and education, and six questions about VR education.
Data analysis
The results are expressed as frequency and percentage. The collected data were verified at the significance level of 0.05 using IBM SPSS Statistics ver. 21 (IBM SPSS Inc., Armonk, NY, USA). The chi-square test was conducted to investigate the relationship between sex, academic background, institutional type, clinical experience according to the presence or absence of VR education, and necessity of VR education. The reliability of the questionnaire was high (Cronbach alpha=0.77) in the category related to VR education.
RESULTS
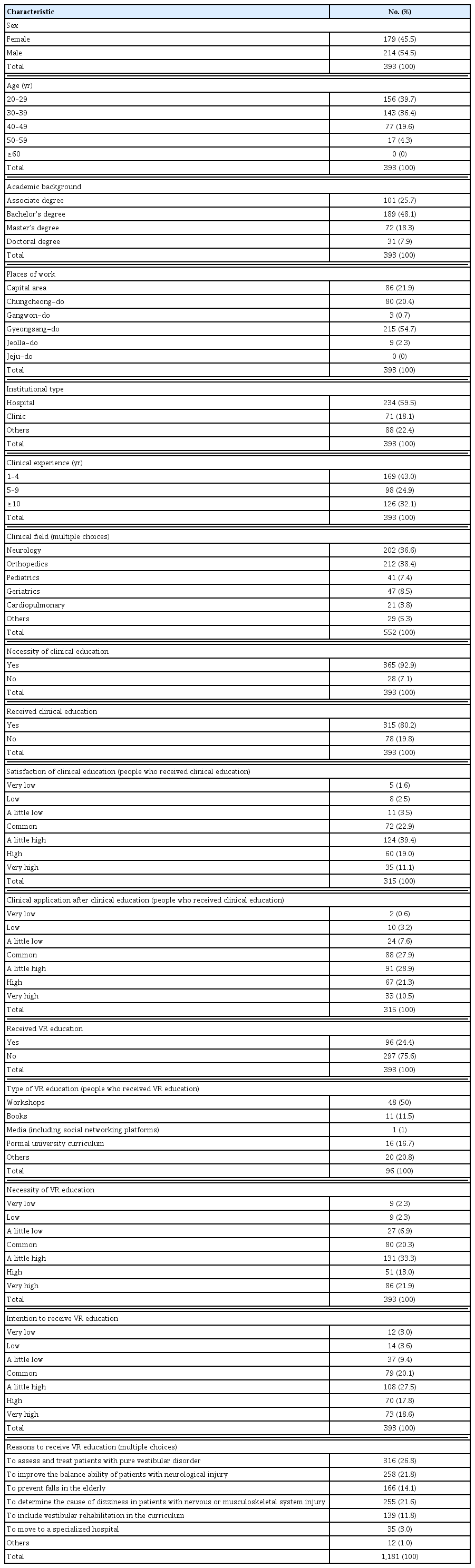
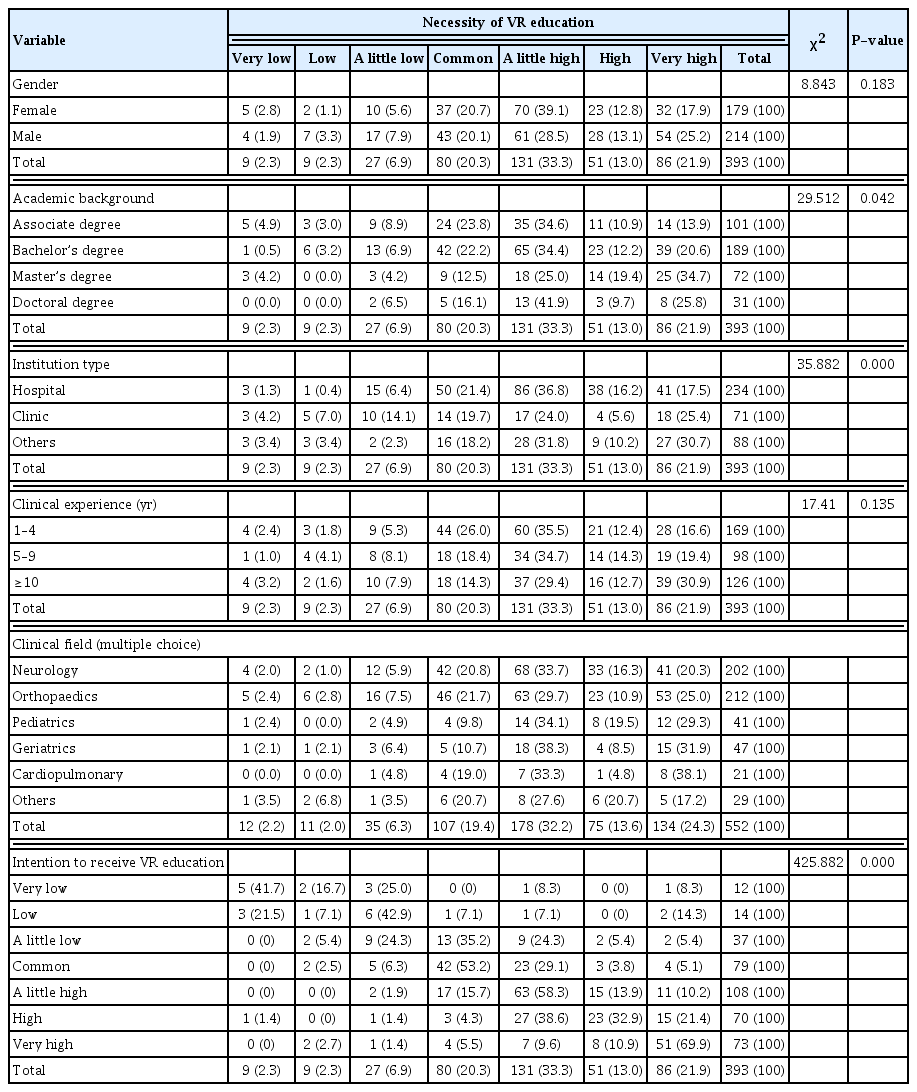
Table 1 showed general characteristics of respondents. There was no statistically significant difference in the sex, academic background, institutional type, and necessity of VR education according to the presence or absence of VR education (P>0.05). However, there was a statistically significant difference in clinical experience and intention to receive VR education according to the presence or absence of VR education (P<0.05). Among those who had VR education, most worked in the field of neurological physical therapy, and those who did not mainly worked in the field of orthopedic physical therapy. Those who had VR education participated mainly in workshops (50%). Regarding the reasons for attending VR education, most of those who did or did not have VR education answered that they would attend “to assess and treat patients with pure vestibular disorder,” “to improve the balance ability of patients with neurological injury,” and “to determine the cause of dizziness in patients with nervous or musculoskeletal system injury” (Table 2).
There was no statistically significant difference in the sex and clinical experience according to the necessity of VR education (P> 0.05). However, there was a statistically significant difference in academic background, institutional type, and intention to receive VR education according to the necessity of VR education (P<0.05). The reasons for “VR education is necessary” included: “Many patients complain of dizziness, but I do not know how to treat,” “Incidence of falling increases as the elderly population increases,” “I want to provide various interventions for patients with poor balance and walking ability,” and “I want to learn because I do not know what VR is.” The respondents believed that VR education was needed to enhance the diversity, access, and expertise of the physical therapy field. Furthermore, they answered that the necessity of VR education was more than “a little high” in all clinical fields (Table 3).
DISCUSSION
The present study suggests the urgent need of professional education for VR and the cooperation and attention of related medical staff in Korea. Most respondents with a clinical experience of >10 years answered that they had received VR education, whereas most of those with <5 years of clinical experience responded that they did not. Physical therapists treat many patients with various diseases as their clinical experience increases. It is speculated that experiences that did not solve the problems of patients with dizziness led to need for VR education. Thus, these circumstances may have played a role in understanding the importance of VR education. However, regardless of their clinical experience, most respondents answered they had no VR education. Most physical therapists who responded to this survey treated patients with neurological or musculoskeletal injuries, possibly because many physical therapists focus mainly on the curriculum to understand the diseases and learn to treat them. Furthermore, physical therapists are enhancing their capabilities through professional education (neurological or orthopedic physiotherapy courses, about 120–350 hr) to become experts in their fields after graduation (Korea Proprioceptive Neuromuscular Facilitation Association, 2020; Korean Academy of Orthopedic Manual Physical Therapy, 2020; Korean Bobath Association, 2020). Our study also found that 80.2% of the respondents had professional education, which is believed to develop professional ability by changing medical environment and increasing awareness of people’s right to knowledge. Thus, Korean physical therapists who are less likely to treat patients with vestibular disease may have been relatively less interested in VR education.
According to a recent Cochrane review, there is moderate-to-strong evidence that VR is a safe and effective treatment for peripheral vestibular disease (McDonnell and Hillier, 2015). In many countries, VR is carried out by otolaryngologists, neurologists, rehabilitation physicians, and physical therapists. The American Physical Therapists Association has published clinical guidelines for VR for peripheral vestibular diseases (Hall et al., 2016). However, in Korea, VR is executed by doctors, nurses, and audiologists. After that, handouts are provided for patients to exercise at home (Kim, 2013; Lee et al., 2011). Recently, Lee and Choi-Kwon (2016) reported that the implementation rate of self-home exercise for patients with peripheral vestibular disease was very low. Many researchers reported that individualized VR tailored by a physical therapist was more effective than general VR (Gottshall, 2011; Norré and Beckers, 1988; Sessoms et al., 2015) because physical therapists play an important role in directly restoring patient function and return to daily life by identifying the patient’s specific impairments and functional limitations. In addition, because physical therapists have been in continuous face-to-face contact with patients for a long time, they have a significant impact on patients’ functional recovery as well as emotional well-being (Cho, 2008; Eleftheriadou et al., 2012; Shim et al., 2008; Shin and Cho, 2019). Nevertheless, physical therapists in Korea are not participating in VR because of the following reasons: insufficient cooperation among clinicians in rehabilitation medicine, otolaryngology, and neurology and absence of insurance-related items (Kim, 2013; Rhee et al., 2006). It is speculated that these factors have led to the lack of understanding of VR among physical therapists in Korea. It has led to the need for VR education. In the present study, respondents recognized a high positive response for the necessity of VR education without received VR education. However, currently, VR is not introduced in the clinical sections provided by the Korean Physical Therapy Association (2020).
Recently, the customized vestibular exercise, proposed by otolaryngologists, has been recognized as a new medical therapy (National Evidence-based Healthcare Collaborating Agency, 2020). VR is introduced through conservative education conducted by the Korea Physical Therapy Association and workshops by a special academy. Therefore, many physical therapists have stated showing interest in VR. In the present study, most of the respondents answered positively to the question “Would you attend if VR education is held?” Those who answered positively to the necessity of VR education also showed a positive intention to receive VR education. The main reasons for attending VR education were “to assess and treat patients with pure vestibular disorder,” “to determine the cause of dizziness in patients with nervous and musculoskeletal system injury,” and “to improve the balance ability of patients with neurological injury.”
In conclusion, many Korean physical therapists recognize the necessity of VR education. However, there are few experts or organizations that can provide related education. Therefore, related associations, academic societies, and expert groups should develop appropriate education and qualification programs to comply with the needs of VR education in Korea. Certain standards should be established for the organizers and the completion of education. Moreover, because Korean physical therapists do not currently have independent rights to treat rehabilitation patients by medical law, related medical staff will need to cooperate with them and recognize the importance of VR.
Lastly, this study had some limitations. First, it is difficult to generalize the study results due to the small sample size. Second, more information could not be obtained due to fewer questionnaires. Third, studies have no reported on the current status of physical therapists regarding VR in Korea. Therefore, it was difficult to compare the results of this study with those of previous studies. Nonetheless, this study may help to recognize the role and importance of VR to physical therapists in Korea.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.