Therapeutic exercise based on biobehavioral approach for the rehabilitation of a radial nerve injury after surgical removal of a schwannoma: a case report
Article information
Abstract
Schwannoma is a benign tumor located in the Schwann cells of the nerves. A 36-year-old white man underwent surgery after being diagnosed with radial nerve schwannoma of the upper right extremity between the triceps brachii muscle and brachioradialis muscle, after which a complete axonotmesis of the aforementioned nerve trunk occurred. The symptomatology presented by the patient included a loss of both motor and sensory function of the fingers, hand, and right forearm. The treatment was a biobehavioral physiotherapy approach that included therapeutic exercise, neuro-orthopedic manual physical therapy, therapeutic education, and sensitivity retraining. The biobehavioral approach in physiotherapy includes a multimodal approach that encompasses biological aspects, along with cognitive-evaluating and motivational-affective components. Two weekly sessions were held for 6 months, resulting in a total of 48 sessions. Using multimodal physiotherapy based on a biobehavioral approach, after 6 months of treatment, the symptoms improved. The motor function of the upper limb improved considerably due to the recovery of increased activity of the superficial musculature dependent on the radial nerve. However, the functions dependent on deep forearm and hand musculature recovered to a lesser extent. At the sensory level, the retraining of sensitivity allowed the patient to regain an important sensitivity. This case report explains the treatment used and the findings obtained, given a large percentage of the functionality that had been lost was recovered.
INTRODUCTION
Tumor pathology is uncommon in nerve tissues of the upper extremities. Within this unusual pathological presentation, schwannoma is the tumor that occurs most frequently (Kang et al., 2000). Although cases of tumor cell expansion have been described, usually located in the Schwann cells of these nerves, schwannoma is a benign tumor (Kang et al., 2000).
The usual treatment performed to remove the neoplasm is surgery, which aims to remove the tumor cells present in the Schwann cells while attempting to maintain the maximum integrity of the affected nerve, thus obtaining a good prognosis in these cases. However, surgery is not always optimal because structural injury to nerve tissue has sometimes been reported after the surgery, requiring repair (Kang et al., 2000). With regard to surgical treatment, sometimes the tumor contains a capsule that can encompass all, or some nerve fibers with what is usually performed a microsurgery of “shelling out.” Afterwards, an autologous autograft is usually performed using other peripheral nerves such as the sural nerve or the medial cutaneous arm nerve with the aim of restoring the continuity of the nerves (Kang et al., 2000).
These kind of complex situations require a biobehavioral approach, because the influence of both the affective-emotional such as kinesiophobia, depressive symptoms or anxiety and the cognitive-evaluating variables such a catastrophic thoughts, bad expectations, low self-efficacy beliefs, or erroneous beliefs could act as a barrier to patient recovery (Cuenca-Martínez et al., 2018; Gil-Martinez et al., 2018; Turk, 2003; Turk and Okifuji, 2002). The biobehavioral approach aims to improve the patient’s motivation, change their beliefs and misconceptions, increase the locus of internal control, and maintain adherence to treatment (Beltran-Alacreu et al., 2015a; Turk, 2003). Beltran-Alacreu et al. (2015a) found that a biobehavioral-based multimodal physical treatment produced a substantial reduction in pain intensity, pain catastrophizing, disability and the impact of headaches in a patient with chronic tension-type headache. In addition, Grande-Alonso et al. (2019) recently showed that physiotherapy based on a biobehavioral approach, with or without orthopedic manual physical therapy, was effective in the treatment of nonspecific chronic low back pain until at least 3 months after receiving the intervention. Similar results were also obtained by Beltran-Alacreu et al. (2015b).
This case study describes the evaluation and development of a multimodal physiotherapy treatment based on a biobehavioral approach in the rehabilitation of a radial nerve injury after surgical removal of a schwannoma. This is the first case study assessing a biobehavioral physiotherapy treatment in a patient with radial nerve schwannoma. The authors thought this approach was necessary because the patient was referred from several care centers without obtaining significant improvements. The treatment the patient previously received was a classic physiotherapy treatment based on electrotherapy and massage (usual care). It is therefore that the purpose of this study was to evaluate and treat a patient with a nerve injury through a biobehavioral approach based on the patient-centered biopsychosocial model.
MATERIALS AND METHODS
Case history
The patient was a 36-year-old white man (weight, 70 kg; height, 178 cm) who underwent surgery after being diagnosed with radial nerve schwannoma of the upper right extremity between the triceps brachii muscle and the brachioradialis muscle, after which a complete axonotmesis of the aforementioned nerve trunk occurred. The axonotmesis was later repaired by a bifascicular autograft of the sural nerve. A calendar of the patient’s previous history is shown in Appendix 1.
The main symptomatology presented by the patient during the initial interview was a loss of both motor and sensory function of the fingers, hand, and right forearm, together with the presence of burning pain in the area of the forearm and a sense of tightness. The patient underwent a nerve conduction study at 3 and 6 months after the second surgery, in which the results of complete axonotmesis were found, with no evidence of ongoing reinnervation.
Clinical findings
In relation to the physical therapy evaluation, the abolition of the motor response was observed in the form of loss of muscular mass of the upper right extremity. The burning pain sensation was located on the dorsal side of the forearm.
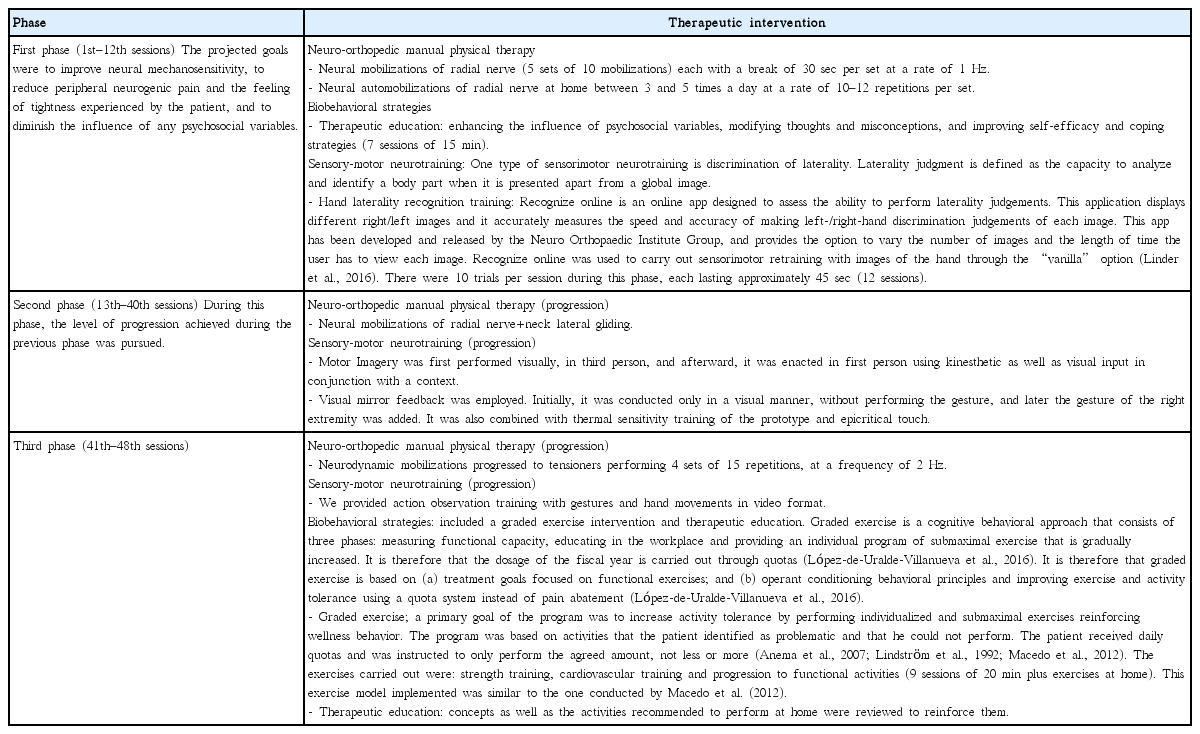
With regard to range of motion (ROM), a significant loss of active ROM was observed, given evident denervation of the musculature attributed to the radial nerve. The ROM was decreased in all movements of the forearm, wrist and fingers with the exception of the elbow pronation movement. A decrease in active ROM was found in wrist extension, wrist flexion, wrist abduction, wrist adduction, elbow supination, thumb abduction, thumb extension and fingers (second, third, fourth, and fifth finger) extension, which were in a fallen position. All baseline measurements (T0) of the active ROM in the affected upper limb are found in the Table 1. The ROM was measured through a mobile application consisting of a digital goniometer, whereas the movements of pronation and supination were measured with a hand goniometer (Pourahmadi et al., 2017).
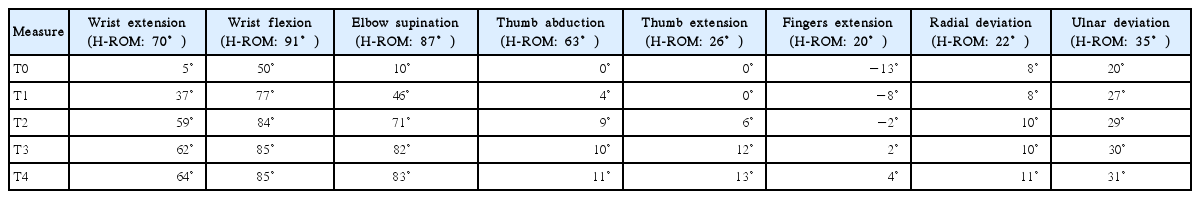
Baseline and follow-up measurements of the active range of motion in the affected upper limb from T0 to T4
In terms of diagnostic tests, a neurodynamic test of the radial nerve (ULNT 2B) was performed and very low mechanosensitivity was found. The neurodynamic tests on the median nerve (ULNT 1) and ulnar nerve (ULNT 3) showed no relevant findings. In the somatosensory assessment, the 2-point discrimination test was evaluated in the sensitive region corresponding to the radial nerve, both on the healthy side and on the affected side, with an esthesiometer (Nolan, 1982). The main finding was that no response was found in the 2-point discrimination test in the sensitive territory corresponding to the radial nerve of the affected upper limb. The minimum distance where the healthy upper limb could discriminate was 3 cm (Table 2).
Finally, a set of self-report questionnaires was given to the patient concerning psychosocial issues, pain, function, and disability: the Spanish version of the pain catastrophizing scale (PCS) to assess the degree of pain catastrophizing, the pain intensity was measured using a numeric pain rating scale (NPRS), the Spanish version of the Hospital Anxiety and Depression Scale, and the Spanish version of QuickDASH (disability of the arm, shoulder, and hand) to evaluate the symptoms and physical disabilities of the patient.
The Spanish version of the PCS assesses the degree of pain catastrophizing. The PCS has 13 items and a 3-factor structure of rumination, magnification, and helplessness. The highest score on this questionnaire is 52. Higher scores indicate higher levels of catastrophic thoughts (García-Campayo et al., 2008).
Pain intensity was measured using a NPRS. The NPRS is a segmented numerical version of the analogue visual scale consisting of 11 points, and it ranges from 0 representing “no pain” to 10 representing “worst pain imaginable” (Ferraz et al., 1990).
The Spanish version of hospital anxiety and depression scale (HADS) consist of a 14-item instrument with a 4-item Likert scale that measures from 0 to 3. This instrument has two subscales consisting of seven items each. Both the anxiety and depression subscales have a maximum score of 21 points. Even if it’s the same questionnaire, the subscales work separately. Higher scores on each subscale indicate higher levels of depressive symptoms and anxiety (Quintana et al., 2003).
The Spanish version of QuickDASH evaluates the symptoms and physical disabilities of the patient. This version has 11 questions with five alternatives and a maximum score of five for each question. The QuickDASH questionnaire score has a maximum score of 100. Higher scores indicate greater dysfunctionality of the upper limb (Hervás et al., 2006).
Therapeutic intervention
Two weekly sessions were held for 6 months, resulting in a total of 48 sessions. The biobehavioral physiotherapy approach included therapeutic education, neuro-orthopedic manual physical therapy, therapeutic exercise, and sensitivity retraining. It also encompassed various techniques in neuro-training, such as laterality training, action observation training, kinesthetic motor imagery, and visual mirror feedback. All treatments had a total duration of 30 min spread over 12 sessions. Appendix 2 shows the therapeutic intervention carried put.
RESULTS
The patient received a total of 48 sessions, each consisting of 30 min in duration. Five measurements were taken: the first was basal (T0), the second took place 2 months after starting the treatment (T1), the third at the 4th month of treatment (T2), the fourth at the end of treatment (T3), and the fifth a month after treatment completion (T4). The results obtained are presented in the result tables (Tables 1, 2).
The motor function of the upper limb improved considerably due to the recovery of increased activity of the superficial musculature dependent on the radial nerve (brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis, and elbow supinator muscles). The patient reached 85° of active wrist flexion, 64° of active wrist extension, and the total degrees of wrist abduction and adduction was 42°. However, the functions dependent on deep forearm and hand musculature recovered to a lesser extent. At the sensory level, the retraining of sensitivity allowed the patient to regain an important sensitivity such as the ability to respond to an alarm signal (protective function). Nevertheless, this somatosensory recovery was not complete because the subject showed that the minimum distance to discriminate 2 points was 5 cm in the affected upper limb, compared to 3 cm in the healthy upper limb.
DISCUSSION
This case report presents a detailed description of the evaluation and the partially successful evolution of an adult male patient with a complete axonotmesis in the radial nerve which was later repaired by a bifascicular autograft of the sural nerve who was treated with physiotherapy based on a biobehavioral approach. The motor and the sensory functions were partially recovered one-and-a-half years after the repair surgery was undertaken. These functions remained completely nonresponsive after surgery, as shown both in the postintervention measurements and in a nerve conduction study.
The brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis, and supinator muscles function were recovered practically in its entirety, whereas the intermediate and deep musculature recovered only partially (extensor digitorum, extensor digiti minimi, abductor pollicis longus, extensor pollicis, extensor pollicis longus, extensor pollicis brevis, and extensor indicis). Based on the study of Ryu et al. (1991), the most clinically relevant finding was that 40° of wrist extension, 40° of wrist flexion, and a total of 40° of radial-ulnar deviation is needed to perform a majority of the activities of daily living. These results were achieved in the present case study. These improvements were objectified through the QuickDASH questionnaire, which showed a substantial improvement after the intervention.
Neural mobilization, which has shown to promote neural regeneration after peripheral neurogenic injury, was key in the treatment, as were the techniques aimed at provoking cortical reorganization by improving the motor function (e.g., motor imaging and visual mirror feedback) (da Silva et al., 2015). The study conducted by Villafañe et al. (2013), found similar results to those obtained in the present study, where a program with manual therapy and neurodynamic mobilization improved the function of a patient with peroneal nerve paralysis.
At a sensory level, sensitivity retraining allowed the patient to recover some important sensitivity, such as the ability to respond to an alarm signal. The patient had previously suffered burns in the previous rehabilitation centers due to anesthesia in the affected area. Therapeutic education made it possible to reduce the influence of psychosocial variables while improving adherence to treatment, increasing self-efficacy, and improving the motivational aspect. This could be observed through the obtained scores in the self-reported HADS and PCS questionnaires, where their influence practically ceased after the intervention. Therapeutic education has shown similar improvements within a multimodal physiotherapy program in different clinical entities (Beltran-Alacreu et al., 2015b; Kindelan-Calvo et al., 2014). The lack of scientific evidence on a biobehavioral approach for this pathology does not allow us to compare our results with other authors. However, Engquist et al. (2013), using a multimodal physiotherapy treatment based on the biobehavioral approach, showed positive long-term results in patients with cervical radiculopathy.
Clinically, a multimodal physiotherapy based on a biobehavioral approach seems to offer solutions in the biological sphere, but also in cognitive-emotional aspects widely present in complex patients. The use of sensorimotor neurotraining tools may be interesting in patients who have suffered a prolonged disuse of some body area. Therapeutic education should be used by clinicians to improve adherence to treatment, as well as to improve the negative influence of some psychosocial variables such as catastrophic thinking, low self-efficacy, poor expectations, erroneous beliefs, etc. Finally, the neurodynamic technique may be an interesting tool for problems related to altered mechanosensitivity of a peripheral nerve although further research is needed to clarify some aspects.
The present study presents several limitations that should be taken into account. First, since a nerve conduction study could not be performed (at postintervention), there are only indirect evidences of reinnervation of the radial nerve-dependent musculature. The increase of the active ROM and the improvement of the functionality of the affected upper limb are considered as such indirect evidences. Second, it would have been interesting to collect data on the grip strength of the hand in order to compare the results before and after the intervention. Third, changes in cortical reorganization caused by different sensorimotor neurotraining tools such as kinesthetic motor imagery, action observation training or visual mirror feedback must be considered as a hypothesis because no neuroimaging technique confirming this speculation was used in the present case study. In addition, it is important to stress the fact that there were so many types of interventions. When this occurs, it is difficult to establish attributions about which intervention contributed the most to the patient’s improvements. Finally, due to the fact that it is a case study, it is impossible to establish comparisons. It is possible that the patient’s natural history could have influenced the patient’s improvements; however, the authors believe there is strong evidence to think that the treatment had a significant impact on the patient’s recovery.
ACKNOWLEDGMENTS
The authors thank the Instituto de Rehabilitación Funcional (IRF) La Salle and the Centro Superior de Estudios Universitarios (CSEU) La Salle for making this study possible.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.