The effect of cardiac rehabilitation at 4 weeks postoperatively on quality of life in patients treated with totally thoracoscopic ablation
Article information
Abstract
There is a lack of evidence on the effect of exercise-based cardiac rehabilitation (EBCR) in patients treated with total thoracoscopic ablation (TTA) for atrial fibrillation (AF). Our study investigated the efficacy and safety of postoperative exercise intervention in patients recovering from TTA. Twenty-four patients participated in the study, and were divided into the two groups, exercise group (EG) (n=12) and control group (n= 12). Patients in EG performed the exercise intervention including the aerobic and resistance exercise program twice a week for 8 weeks, which was used as a hospital-based cardiac rehabilitation for the out-patient. A cardiopulmonary exercise test was administered to evaluate aerobic exercise capacity, and qualitative aspect of patient’s life was assessed using the Short Form 36 questionnaires to compare pre and postoperative wellness of patient’s life. Although there was an increase of VO2peak (peak oxygen uptake) after exercise intervention, no significant improvement was found (P=0.055). Two of 4 physical health scores (role-physical, P=0.013 and general health, P=0.05) and three of four mental health scores (vitality, P=0.027, social function, P=0.016, and mental health, P=0.003) were significantly improved after 8 weeks of EBCR. Each summarized scale in the physical (P=0.022) and mental (P= 0.004) survey section was also significantly improved in postoperative assessment compared to the preoperative one. In this context, we concluded that EBCR initiated at the time point of 4th week after TTA operation can guarantee the secure postoperative physical activity, and the 8 weeks of EBCR can effectively improve the quality of life in AF Patients.
INTRODUCTION
Atrial fibrillation (AF) is a common arrhythmia, and has been known to occur in the general population by approximately 0.4% (Chugh et al., 2014). Study reported that AF can increase incidence rate of stroke by 3–5 times (Wolf et al., 1978). Early prophylactic intervention such as antiarrhythmic therapy controlling heart rate or cardiac rhythm was considered as a primary treatment for AF (Camm et al., 2012). Based on the medical guidelines for the AF, surgical modalities such as the catheter and radio-frequency ablation showed a satisfactory outcome compared to the pharmacological treatments (Camm et al., 2012). In this context, conventional surgical approach was still thought to derive beneficial prognosis and clinical outcomes in restoring the abnormal sinus rhythm affected by AF.
The total thoracoscopic ablation (TTA) was a well-recognized surgical option for the AF, which ablates the lesion by applying a minimally invasive technique (Vos et al., 2018). After TTA administration, exercise-based cardiac rehabilitation (EBCR) has been known as a clinically prospective application to the AF patient, and had a positive effect on improving the exercise performance and wellness of life in AF patient (Hegbom et al., 2007; Reed et al., 2013). It was reported that, in AF patient, the cardiopulmonary fitness characterized with peak oxygen uptake (VO2peak) is 20% lower than the age-matched general population, and is associated with the mortality and survival rate of AF patients (Pardaens et al., 1997). Studies showed that when the EBCR was applied to cardiac patients, exercise-related performance was improved after the catheter surgery and cardiac ablation (Aliot et al., 2014; Fengsrud et al., 2016).
Although the wellness of life in AF patients was likely to be lower than age-matched general population, cardiac rehabilitation combined with physical activities was thought to significantly improve the qualitative aspect of patients suffered from sinus arrhythmia (Aliot et al., 2014). Since most studies (Aliot et al., 2014; Hegbom et al., 2007; Reed et al., 2013) intensively focused on the solely therapeutic and surgical approach, the application of EBCR was not emphasized enough as a possible clinical intervention. One study reported that the mental health in patients undergoing the endoscopic ablation could be improved through the application of EBCR (Fengsrud et al., 2016). Moreover, another study suggested that 12 weeks of EBCR could enhance the physical performance, but not in the wellness of life, particularly in mental health.
TTA is a surgically secure approach, and results in less complication rate in the early-recovery period (Vos et al., 2018). However, at the one year of surgical follow-up, one study found that AF recurred after the thoracoscopic ablation by 6.3%; the risk factors for the AF were age, hypertension, and left atrial volume index (On et al., 2015). Additionally, considering that patients treated with TTA may be reluctant to conduct the physical activities due to the sense of insecurity regarding the exercise-induced recurrence of AF, clinically proved safe period to perform the EBCR will be an important consideration that can ameliorate the exercise performance and wellness of their life in AF patient.
There have been limited studies regarding the effect of EBCR on exercise capacity in AF patient treated with the surgical intervention. Therefore, the purpose of our study was to assess the effect of 8 weeks EBCR initiated at the time point of 4th week after TTA operation on the cardiopulmonary fitness and quality of life (QoL) in patients treated with TTA.
MATERIALS AND METHODS
Study design
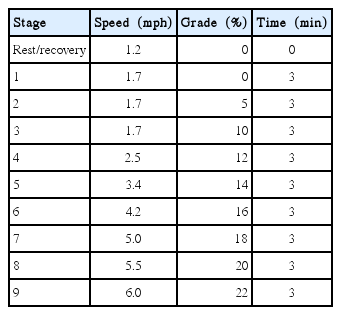
Twenty-four patients treated with TTA participated in this study. All patients performed a cardiopulmonary exercise test, and electrocardiogram (EKG) was also recorded by 10 electrodes. The wellness of patient’s life was assessed by means of the Korean version of Short Form 36 Quality of Life questionnaires (Han et al., 2004). After the baseline test, the patients were divided into the two groups on the basis of the patient’s willingness to participate in performance test: exercise group (EG) (n=12) and control group (CG) (n=12). The CG had only medication treatment, and patients showing AF recurrence after surgery were excluded from our study design. The study was approved by the Institutional Review Board of Samsung Medical Center (IRB No. 2018-04-060-001). The patients conducted the incremental treadmill exercise test equipped with respiratory gas exchange analysis (Parvo Medics, East Sandy, UT, USA), and the primary outcome of this study was exercise capacity, VO2peak. VO2peak defined as the maximum oxygen consumption was measured in preintervention (4th week after the surgery) and postintervention (12th week after the surgery) period. The test was maintained for 8 and 12 min on the treadmill and started at a speed of 1.7 km/hr with 0% incline according to modified Bruce protocol by Samsung Medical Center, which was optimized protocol for the cardiac patient (Table 1). During the rest and test period, physiological responses including heart rate, blood pressure, rate-pressure product, and respiratory exchange ratio were measured as well. The incremental exercise test was conducted through the guidance of American College of Sports Medicine (American College of Sports Medicine, 2010).
Quality of life
Before and after 8 weeks EBCR intervention, the wellness of life in patients was assessed by using the Short Form 36 questionnaires that have been extensively validated among AF patients (Aliot et al., 2014). Each summary of two major scales (physical and mental health section) was scored and standardized to compare each subject, and the higher score in questionnaire indicates the improvement in QoL.
Exercise program
The EG started the exercise intervention at the time point of 4th week after surgery, and all patients in EG participated in the exercise program that was administrated based on the frequency, intensity, time, and type of exercise. The EG performed 16 exercise sessions consisting of aerobic and resistance program twice a week for 8 weeks. Patients’ EKG during the exercise program was monitored by the Q-Tel (Quinton, Bothell, WA, USA). Each training session was conducted for 1 hr with 5 min of warm-up and cool-down period. Using the result of cardiopulmonary exercise test, 40%–50% of heart rate reserve (HRR) was applied as an initial aerobic exercise intensity, which was progressively increased to 75% of the HRR during the 8-week exercise program period. For the resistance training in EG, weight-loaded machines were used after the 2 weeks of aerobic exercise, and 2–3 sets with 10–15 repetitions were set as exercise intensity. During the administration of exercise program, the participants were also encouraged to actively perform the treadmill and stationary bike exercise at the S Sports Medicine Center. The initial time for aerobic exercise was 10 min until the 3rd session, which was gradually extended to 30 min per session until at the end of the study.
Statistical analysis
All statistical analyses were performed by IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). Two-way repeated analysis of variance was used to compare the two groups, and comparison between pre and postoperative outcomes was analyzed through the post hoc paired t-test. All data were presented as mean±standard deviation for the data analysis. All statistical significance level was set at P<0.05.
RESULTS
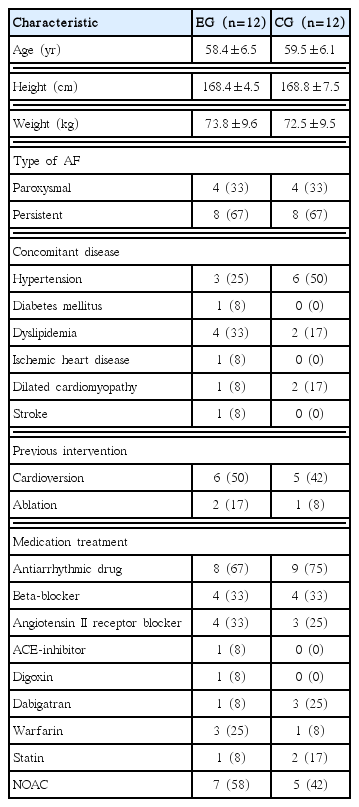
Among 30 patients undergoing TTA surgery in Samsung Medical Center, 24 subjects were finally included in our study (Table 2). After 8-week exercise intervention, there was no statistically significant difference in the VO2peak between the two groups (P=0.90). The exercise intervention induced the improvement of VO2peak, however, no statistically significant interaction effect was found between Group and Time (P=0.055). The VO2peak in the preoperative test was 26.0 and 28.3 mL/kg/min in EG and CG, respectively. After the exercise intervention, EG showed an increased peak VO2 by 28.9 mL/kg/min while CG had a decreased value by 26.9 mL/kg/min.
In the physical health scores, the role-physical (P=0.013) and general health (P=0.050) showed significant interaction effect between Group and Time. The summarized scale in physical survey section also suggested a significant difference in the interaction between group and time (P=0.022) In the EG, role-physical (P= 0.000), and general health (P=0.019) showed a significant improvement compared to the preoperative period. However, physical function (P=0.167) and bodily pain (P=0.537) did not significantly difference in the interaction between group and time (Table 3).
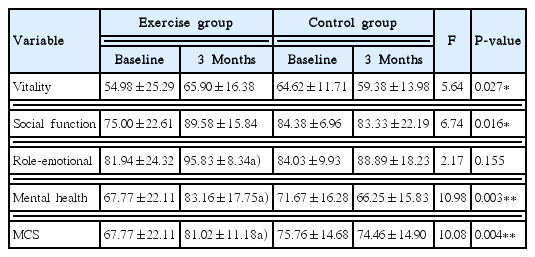
With respect to the mental health scores, a significant interaction effect between Group and Time was found in the assessment of vitality (P=0.027), social function (P=0.016), and mental health (P=0.003). After the 8-week EBCR, there was a significant improvement in the score of social function (P=0.019) and mental health (P=0.011). The summarized scale in mental survey section also showed a significant difference (P=0.004) in the interaction between group and time. However, role-emotional in pre-intervention (4th week after the surgery) did not significantly differ from the post-intervention (12th week after the surgery) (P=0.155) (Table 4).
DISCUSSION
VO2peak known as a cardiopulmonary capacity can be defined as a physiological capability to transport the oxygen to working skeletal muscles during the physical activity. In this scientific sense, the exercise capability in patients suffering the AF has been known to be lower compared to the age-matched population so that improvement in VO2peak was associated with approximately 20% reduced mortality in AF patient (Pardaens et al., 1997). Since AF was considered to impair the ‘atrial kick’ as well as the reservoir and conduit function of the left atrium, it can cause the potential underfilling phenomenon of the left ventricle (Nicod et al., 1986). Moreover, the malfunction of ‘atrial kick’ may impede the cardiac output in patient diagnosed as mitral stenosis, but not in the asymptomatic population (Benussi and de Maat, 2018). In our study, considering the AF patients undergoing TTA may hypothetically have less efficient cardiopulmonary fitness level compared to age-matched population, it is speculated that their skeletal muscle function for physical activity will be negatively impacted by precarious VO2peak.
In our investigation, VO2peak was increased by 19% after the EBCR, which, however, was not statistically significant. This finding is in agreement with a systematic review research (Reed et al., 2013), but these scientific concepts simultaneously demonstrated the less beneficial effect of short-term exercise intervention in patients having the AF. On the other hand, another study (Hegbom et al., 2007) found that 8-week short-term intervention improved the exercise performance and wellness of life in AF patients. Considering that technically different ablation surgery and different exercise programs were administered in the independent study, the improvement of VO2peak may depend on each research condition and design. Compared to previous studies (Hegbom et al., 2007; Risom et al., 2017) applying the long-term exercise program, since our study had less intensive exercise program for AF patients in terms of frequency and duration, this may result in the teleological consequence nonsignificant improvement of VO2peak.
As the AF patients also frequently experience psychological hardships in their life, medical interventions aimed at the control of heart rate and cardiac rhythm have been known to focus on the improvement of wellness of patient’s life (Aliot et al., 2014). When studies applied the physical activities to AF patients, there was a clinically positive impact that ameliorates the assessment of physical and mental health. In our study, when the Korean version of Short Form 36 questionnaires (Han et al., 2004) was used to evaluate the patient’s QoL, significantly improved physical and general health assessment were identified after the exercise intervention. Other studies (Hegbom et al., 2007; Kato et al., 2017) reported the beneficial effect of physical activity on the wellness of AF patient’s life. As the aforementioned studies (Hegbom et al., 2007; Kato et al., 2017) demonstrated that physical activity or TTA surgical application can play a pivotal role in promoting the sense of postoperative life satisfaction, the clinical combination of physical activity and surgical administration defined as EBCR needs to be verified whether EBCR could be possible method for patients with AF. Using EBCR, although a significant increase of VO2peak was not found in our study, EBCR initiated at the time point of 4th week after TTA could significantly improve the QoL in AF patients.
Although TTA surgical intervention can be a medically feasible application providing the low complication rate (Vos et al., 2018), 6.3% of AF recurrence rate was reported after 12 months of TTA (On et al., 2015), and physical activity was considered to be associated with the occurrence of AF (Mont et al., 2008). However, recurrence AF and AF-related complication did not occur during the exercise intervention period when patients participated in EBCR 1 month after TTA surgery. In conclusion, based on our results, 8 weeks of EBCR can provide favorable opportunities to AF patients undergoing TTA in respect of enriching the wellness of their life. More importantly, it is found that the EBCR initiated at the time point of 4th week after the TTA surgical operation can be clinically secure and effective intervention for AF patients.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.