Effects of linear versus nonperiodized resistance training on isometric force and skeletal muscle mass adaptations in sarcopenic older adults
Article information
Abstract
The aim of this study was to compare the effects of linear periodization (LP) versus nonperiodized (NP) resistance training on upper-body isometric force and skeletal muscle mass (SMM) in sarcopenic older adults. Twenty sarcopenic older adults were randomly assigned into the LP and NP groups and performed 16 weeks of resistance training. The SMM was measured by octopolar bioelectrical impedance. The isometric force for handgrip and trunk were assessed by dynamometer. Evaluations were performed at baseline, after 4, 8, 12, and 16 weeks of resistance training. For total weight lifted, there was a main effect for time (F=126.986, P<0.001), statistically significant difference between condition (F=13.867, P=0.001) and interaction (F=8.778, P<0.001), whereby total weight lifted was greater for NP after 4 months of training. Isometric force for handgrip and trunk increased across time (P<0.001) but no significant differences between groups or interaction were observed (P>0.05). The SMM increased across time (P<0.05), however no significant difference between groups or interaction were observed (P>0.05). There were strong and significant correlations between handgrip maximum force and SMM (LP: rho=0.79, P=0.004 vs. NP: rho=−0.43, P=0.244) and handgrip mean force and SMM (LP: rho=0.68, P=0.021 vs. NP: rho=−0.37, P=0.332) only for the LP group. In conclusion, LP and NP resistance training induced similar benefits on upper-body isometric force and SMM in sarcopenic older adults. However, LP presented lower total weight lifted, suggesting that it is possible to obtain similar gains in isometric force and SMM with less total work.
INTRODUCTION
The aging process is characterized by decreases in the physiological functions of several organ systems and tissues (López-Otín et al., 2013). One of the most affected tissues with aging is skeletal muscle mass (SMM), where atrophy that occurs as a result of disuse, poor nutrition, and a myriad other factors is accentuated (Aniansson et al., 1986; Nilwik et al., 2013). This condition can be defined as sarcopenia, in which the muscle mass index (SMM/height2) is two standard derivations lower than the mean of healthy adults (Curcio et al., 2016). Sarcopenia has been reported to affect 5%–13% of people over 60 years of age and up to 50% of people over the age of 80 (von Haehling et al., 2010). The loss of muscle mass has been traditionally associated with reductions in functional capacity, impaired mobility, loss of independence, and an increased risk of falls and factures (Alley et al., 2014; Lindemann et al., 2016; Manini et al., 2007). However, more recent research demonstrates that during aging muscular strength is lost at a rate of approximately 3–4 fold greater than muscle mass (Mitchell et al., 2012), which suggests that neuromuscular changes affecting muscular strength likely mediates much of the relationship between sarcopenia and reduced mobility (Visser et al., 2005). Muscle mass, on the other hand, serves important physiological functions, including providing a protein reservoir necessary to withstand disease conditions and to maintain plasma amino acid concentrations, glucose and fatty acid metabolism and disposal, and the maintenance of bone mass (Wolfe, 2006). Therefore, it seems pertinent to study interventions that simultaneously increase muscular strength and mass in the aging populations.
Resistance training is considered an efficient mode of physical exercise to induce gains in muscle mass, strength and functional capacity in older adults (Hunter et al., 2004; Liu and Latham, 2009; Nilwik et al., 2013) and is therefore recommended to attenuate the effects of sarcopenia in older adults (Aagaard et al., 2010; Roth et al., 2000). To potentiate the adaptations associated with resistance training, practitioners and sport scientists often manipulate training variables, such as volume, intensity, and intraset rest periods via the periodization of training. Periodization can be defined by the process of organizing a training program aiming to achieve peak physical performance while at the same time minimizing the risk of injures and overtraining (Cunanan et al., 2018).
Among the different methods of organizing training is traditional or linear periodization (LP), characterized by a progressive reduction in training volume (repetitions) while increasing the training intensity (load) in the context of resistance training (Issurin, 2010). In young adults, a recent meta-analysis demonstrated that periodization promoted superior strength gains when compared with nonperiodized (NP) training protocols (Williams et al., 2017), however, it is currently unclear as to whether these superior gains in strength are the result of variations in training stimuli inherent to periodization or specificity of training as most NP protocols have been conducted in the 8 to 12 repetition range.
The strength and body composition effects comparing periodization to NP, or between different models of periodization in older adults, requires further investigation. DeBeliso et al. (2005) analyzed the effects of 18 weeks of twice-weekly NP resistance training with a set intensity of 9 repetition maximum (RM) versus LP encompassing 6-week blocks of 15 RM, 9 RM, and 6 RM on strength gains in untrained older adults. Both protocols induced similar increases in maximum strength, measured via one-repetition maximum tests. In another study, Conlon et al. (2016) compared the effects of three different models of periodized training (linear, undulating, and NP) conducted 3 times per week for 22 weeks per week in older adults, and concluded that all three models of training promoted equal improvements in lipid profile, systolic blood pressure, maximal isometric strength, functional capacity, balance confidence, and body composition.
Despite several studies having analyzed the effects of resistance training with different periodization protocols in young adults (Kraemer et al., 2003; Monteiro et al., 2009; Moraes et al., 2013) and older adults (Conlon et al., 2016; DeBeliso et al., 2005), there are a lack of studies that have investigated the effects of LP versus NP training on strength and muscular adaptations in sarcopenic older adults. Understanding the effects of different resistance training protocols is of importance to fitness and healthcare professionals working with sarcopenic people, since lean body mass and strength are important, modifiable indicators of mortality (Bunout et al., 2011), and because the global life expectancy continues to increase.
Therefore, the purpose of this study was to analyze the effects of LP versus NP resistance training on upper-body strength and SMM gains in sarcopenic older adults, and to verify the relationship between strength and SMM adaptations in this population. We hypothesized that linear periodized resistance training would be more efficient than nonperiodization to improve upper-body strength and SMM in sarcopenic older adults.
MATERIALS AND METHODS
Experimental design
This study was carried out from September to December 2016 at the Department of Physical Education of São Paulo State University, Brazil. The participants were randomly assigned into two groups: LP and NP. Evaluations were performed at baseline, after 4, 8, 12, and 16 weeks of resistance training. At all evaluation time points upper-body isometric force (handgrip and trunk) and SMM were analyzed.
Subjects
The participants in this study were selected from a larger sample through cohort investigation (Fig. 1). The diagnosis of sarcopenia in this larger sample was verified through the evaluation of the appendicular muscle mass (ALST), measured by dual-energy X-ray absorptiometry, and maximal isometric voluntary contraction (MIVC), measured by dynamometry. ALST was obtained from the quantification of the lean and soft tissue of upper and lower limbs, in kg, divided by height, in meters squared (kg/m) (Curcio et al., 2016). The MIVC was obtained in electronic dynamometer through handgrip. For the diagnosis of sarcopenia, the EWGSOP proposal (Cruz-Jentoft et al., 2010) was applied. Fifty older adults with lower values of the sum of z-scores for ALST and MIVC, according to gender, were invited to participate in the RT study. Of these, 20 accepted and were in accordance with inclusion criteria, including: free from disabling chronic advanced stages of cancer, kidney disease on hemodialysis treatment, hospitalization, and ability to ambulate without help. Twenty male and female older adults were selected to participate in this study, randomly divided into LP (age, 73.5±11.5 years; weight, 70.7± 13.9; and height, 157.4±8.3; n=11, 5 male and 6 female) and NP (age, 73.0±6.7 years; weight, 69.3±9.3; and height, 159.9± 8.5; n=9, 4 male and 5 female). The volunteers signed an informed consent to participate in this study. The study was approved by the Ethics Research Group of the Sao Paulo State University, Presidente Prudente Campus (approval number: 2.321.522), according to the norms of Resolution E196/96 of the National Health Council on research involving human subjects.
Procedures
Resistance training protocol
Participants were initially submitted to four familiarization sessions (2 weeks). After this, they performed 16 weeks of resistance training. In the first four weeks, all subjects executed the same protocol (three sets of 12–15 RM with 60–90 sec of rest between sets, 2 days/wk). From the fifth week, the LP group performed 10 RM at weeks 5 to 8, 8 RM at weeks 9 to 12, and 5 RM at weeks 13 to 16. NP group maintained the same repetitions zone (12–15 RM). For both groups, the intensity of the resistance training was controlled through the zone of maximum repetitions. The load was adjusted weekly to maintain the number of repetitions prescribed, according to the (American College of Sports Medicine, 2009). The sets were executed until voluntary exhaustion, and in the case of the participants executing more or less the repetitions prescribed, the overload was adjusted in order to meet the respected training zone (Rossi et al., 2018). The training program was comprised of 8 exercises performed in the following order: chest press, leg press 45°, front pulldown, knee extension, arm curl, leg curl, triceps pushdown, and calf raises. The resistance training was practiced at the gym and the volunteers were accompanied by professional coaches to guarantee correct movements and safety. The participants were instructed not to perform any other type of physical exercise during the period of the study, so only the effect of resistance training can be evaluated. The total repetition and load were recorded for each session to calculated total volume lifted (repetition×load).
Isometric force
The isometric force of the participants was performed at baseline, after 4, 8, 12, and 16 weeks of resistance training and was estimated by electronic dynamometer (Power Din Standard, CEFISE, Nova Odessa, SP, Brazil). Specific accessories were used for each segmental test, according to the recommendations of the manufacturer. The isometric contractions were performed 3 times, lasting 8 sec with 45 sec between repetitions. Maximum and mean force values were recorded (in kg) to determine handgrip and trunk isometric force. First, the participants performed the handgrip test, and the subjects remained seated with the dominant member on the table and angle of elbow flexion between 120° and 150°. After this, participants performed the trunk test, and the participants remained standing with knees fully extended and hip flexion in 120°.
Skeletal muscle mass
The SMM was performed at baseline, after 4, 8, 12, and 16 weeks of resistance training and was estimated by bioelectrical impedance using an octopolar InBody 720 device (Biospace, Seoul, Korea). The InBody 720 uses 8 contact points, 2 in contact with the palm and thumb of each hand and 2 in contact with the front and heel of each foot, allowing to evaluate 4 body mass compartments (total body water, proteins, minerals, and body fat mass). Five segmental impedances (right arm, left arm, trunk, right leg, and left leg) were measured at 1, 5, 50, 250, 500, and 1,000 kHz. The data were electronically exported to Excel using the Lookin’Body 3.0 software (Biospace, Seoul, Korea). All evaluations were performed at the time of the day (in the morning) in a fasted condition to ensure chronobiological control. Participants were instructed to urinate before the measures, refrain from ingesting food or drink in the previous 4 hr, avoid strenuous physical exercise for at least 24 hr and refrain from consumption of alcoholic for at least 48 hr. The bioelectrical impedance device was calibrated each day according to the manufacturer’s recommendations and the exams were performed by the same professional in the pre- and postintervention periods.
Statistical analysis
The data normality was verified using the Shapiro–Wilk test. The Student t-test for independent samples was used to identify similarities at baseline. A 2×5 repeated measures analysis of variance with the Bonferroni adjustment for multiple comparisons was used to compare LP and NP across conditions and time, respectively. For all measured variables, the estimated sphericity was verified according to Mauchly W-test and the Greenhouse–Geisser correction was used when necessary. The Spearman rank correlation (rho) was used to analyze the relationship between SMM and strength. Statistical significance was set at P<0.05. The effect size for total repetitions performed and workload was calculated via Cohen d ([treatment mean–placebo mean]/pooled standard deviation) whereby a value of >0.20 was considered small, >0.50 moderate, and >0.80 large. The data were analyzed using the SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA).
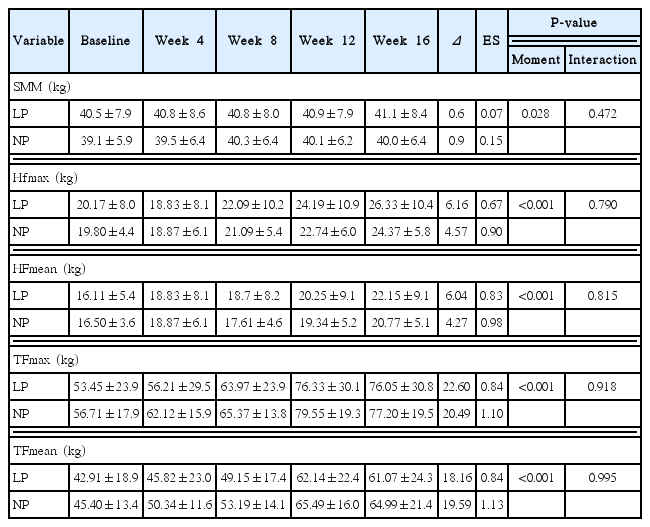
RESULTS
There were no significant differences between groups for age, body weight, height, and strength at the baseline. For total weight lifted (Fig. 2), there was a main effect for time (F=126.986, P< 0.001, η2=0.90), statistically significant differences between condition (F=13.867, P=0.001) and an interaction (F=8.778, P< 0.001). Total volume increased across time for NP and LP, and NP completed significantly more volume than LP after 4 months of training. Table 1 shows the differences in SMM and isometric force performed across time and between groups.

Total weight lifted during resistance training. LP, linear periodization; NP, nonperiodization. aBonferroni post hoc test with P-value <0.05 compared to month-1. bBonferroni post hoc test with P-value <0.05 compared to month-2. cBonferroni post hoc test with P-value <0.05 compared to month-3. *Statistically significantly differences between NP and LP group.
For SMM (F=2.889, P=0.028) there was a main effect of time, however no significant differences between groups or interactions were observed (P>0.05). For maximum handgrip force (F=18.061, P<0.001) and mean handgrip force (F=18.061, P<0.001) there were main effects of time but no significant differences between groups or interactions were observed (P>0.05). For maximum trunk force (F=27.259, P<0.001) and mean trunk force (F= 26.112, P<0.001) there was a main effect of time but no significant differences between groups or interactions were observed (P> 0.05).
In relation to the relationship between SMM changes (Δ after 16 weeks) and isometric force (Δ after 16 weeks) in each group, there were strong and significant correlations between maximum trunk force and SMM (LP: rho=0.79, P=0.004 vs. NP: rho= −0.27, P=0.488) and mean trunk force with the SMM (LP: rho= 0.78, P=0.004 vs. NP: rho=−0.07, P=0.865) only for LP. Regarding to maximum handgrip force and SMM (LP: rho=0.79, P=0.004 vs. NP: rho=−0.43, P=0.244) and mean handgrip force and SMM (LP: rho=0.68, P=0.021 vs. NP: rho=−0.37, P=0.332) there were strong and significant correlations only for LP again.
DISCUSSION
The present study investigated the effect of LP versus NP resistance training for 16 weeks on isometric force gains and muscular adaptations in sarcopenic older adults. The main findings of this study were that LP and NP resistance training promoted similar gains of upper-body isometric force (handgrip and trunk) and SMM. However, LP presented lower total weight lifted, suggesting that it is possible obtain similar gains in isometric force and SMM with less total work. In addition, there was a strong correlation between muscular strength and SMM only for LP.
To our knowledge, this is the first study to investigate the effects of LP versus NP resistance training in a sarcopenic older population. For healthy older adults, there are only a few studies that have compared the effect of periodized resistance training versus NP. Conlon et al. (2016) investigated the effect of 22 weeks of LP, DUP, and NP resistance training on physical function and health in untrained older adults. NP group maintained the same zone of repetition (10 repetitions) during all weeks. The LP group performed 15 repetitions at sessions 1–11, 10 repetitions at session 12–22, 5 repetitions at session 23–33 and equal block in sessions 34 until 60. Daily undulating periodization training was performed in all weeks with 15 repetitions at first session, 10 repetitions at second session and 5 repetitions at third session. The results showed that LP, DUP, and NP promoted similar changes in body composition, lipid profile, systolic blood pressure, maximal strength, functional capacity, and measures of balance efficacy.
Another study analyzed the effect of 18 weeks of LP versus NP resistance training on strength gains in untrained older adults. The LP group performed 15 RM at weeks 1–6, 9 RM at weeks 7–12 and 6 RM at weeks 13–18. NP group maintained 9 RM during all weeks. The authors found similar strength gains in LP and NP group (DeBeliso et al., 2005). In agreement with these studies, Hunter et al. (2001) showed that 25 weeks of DUP and NP resistance training generated equally results on strength and body composition in untrained older adults.
Our results corroborated with the findings of Conlon et al. (2016), DeBeliso et al. (2005), and Hunter et al. (2001), that periodized resistance training promoted similar results compared with NP in untrained sarcopenic older adults. In our study, the LP and NP group experienced similar increases in upper-body isometric force (handgrip and trunk) and SMM. On the other hand, our results also slightly differ from DeBeliso et al. (2005). In DeBeliso et al. (2005) total training volume and average training intensity were equated between groups. This diverges from traditional periodization, including our study, whereby increases in intensity (i.e., from a 9 RM to a 6 RM) are usually matched by decreases in volume. In the present study similar increases in muscle mass and muscular strength were observed despite a significantly lower workload in the LP group. Given reduced work capacities and prolonged recovery periods from resistance training in older adults (Suetta, 2017), our results suggest that periodized resistance training may more efficiently induce neuromuscular adaptations in older adults; however, more research is necessary to verify this hypothesis.
We found a significant relationship between changes in muscle mass and strength only in the LP group. Other studies have reported similar results, in which the increase of muscle strength was significantly correlated with muscle mass gains in older adult populations (Chen et al., 2013; Hayashida et al., 2014). Traditional periodization logic calls for first increasing force production potential by inducing morphological adaptations (i.e., increasing myofibril proteins) through higher repetition training (i.e., 8 to 15 RM), and then to maximize force production per unit of muscle mass by inducing neurological adaptations via high intensity (<5 RM) training (Issurin, 2010). It is interesting that despite no difference in muscle or strength outcomes between groups, a strong relationship between changes in muscle mass and strength were only found in the LP group. Given that there were no interactions and both groups increased across time rather similarly, our results do not support the periodization hypothesis in sarcopenic subjects. Based on these findings, periodization of resistance training in untrained sarcopenic older adults is not necessary to induce superior results in strength and muscle mass gains, demonstrating that in the initial phase of training progressive overload is the most important variable to promote neuromuscular adaptations.
A decrease in SMM in conjunction with reduced neuromuscular potential in sarcopenic people leads to a reduction in muscular strength which ultimately results in a decreased functional capacity, difficulties completing activities of daily living, increased risk of falls and fractures, and lowered quality life (Alley et al., 2014; Lindemann et al., 2016; Manini et al., 2007). Additionally, lean mass is an important indicator of morbidity and mortality (Bunout et al., 2011); therefore, our results highlight the benefits of regular resistance training and emphasize that both models of training could be used as a strategy to increase SMM and strength in sarcopenic older individuals. This study suggests that during the initial phase of training, in untrained older adults, coaches and trainers should focus predominantly on progressive overload to promote adaptations. On the other hand, when coaches and trainers are looking to induce muscle mass and strength gains with less total work, LP may be applied.
The limitations of this study need to be considered when interpreting the findings. The intervention time (16 weeks) may have been insufficient to verify differences between different types of training. Moreover, we can speculate that the variation of load and repetitions in the periodized group was too close to the NP group to promote a different stimulus and, thus, induce divergent adaptations. Therefore, experiments using a wide range of load and repetitions (e.g., 20, 10, and 5 RM) may elicit different results. Thus, we recommend future studies analyze longer periods of training and different periodization programs, including lower repetitions (i.e., 1–4 repetition). Additionally, we cannot directly comment on the transfer of strength in these programs to functional outcomes, and therefore future studies should also assess functional capacity, hemodynamics, and metabolic adaptations. Finally, two nonspecific isometric tests for handgrip and trunk were applied, which could produce lower estimations of muscular strength, as the resistance training program consisted of isotonic exercises and did not train lumbar extension.
In conclusion, 16 weeks of linear or non-periodization resistance training induced similar benefits on upper-body isometric force and SMM in sarcopenic older adults. However, LP presented lower total weight lifted, suggesting that it is possible to obtain similar gains in strength and SMM with less total work in this population. In addition, there were relationships between strength and SMM only for LP.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.