A study on the effect of self bedside exercise program on resilience and activities of daily living for patients with hemiplegia
Article information
Abstract
The purpose of this study was to design a repeatable universal rehabilitation program in which patients with hemiplegia can participate voluntarily, complementing physical and occupational therapies to increase voluntary exercise practice rate. Also, this study attempted to identify the relationship between psychological resilience due to the implementation of self-bedside exercise and functional recovery of activity of daily living (ADL). 12 patients with hemiplegia voluntarily participated in 8 weeks of self-bedside exercise 5 times a day and more than 5 days a week. Their program implementation, resilience, activities of daily living (MBI), upper limb motor functions (MFT), and balance ability (BBS) were analyzed and compared before and after the program. Compared to before implementing the program, significant increases were found in resilience, MBI, BBS, and MFT in the affected side after the implementation, and the resilience scores showed statistically positive correlation in MBI and MFT. Also, the change in resilience before and after the program implementation showed a statistically positive correlation. Therefore, it can be concluded that the self-bedside exercise developed in this study had a positive effect on voluntary participation in exercise as well as resilience and ADL. However, many studies which complement the psychological aspects of hemiparetic patients with stroke are still needed.
INTRODUCTION
Stroke is one of the most common diseases responsible for physical disabilities in Korea (Noh and Shin, 2014), and 70–75% of patients with this disease are not completely recovered. Rather, they experience hemiplegia in which they have to depend entirely on others (Hardie et al., 2004). Hemiplegia not only reduces the ability to maintain adequate muscle tone and posture because of damages in motor skill, sensory channels and its own integrating functions, it also causes difficulties in activity of daily living (ADL) due to various secondary neurological dysfunctions accompanied with problems of motor disorder, sensory disorder, walking difficulty, activity of daily living, and pain (Walker et al., 1999). Stroke mortality is decreasing worldwide whereas its survival rate is gradually increasing. The same phenomenon is also occurring in Korea, which means that the numbers of chronic stroke patients are increasing. In other words, research has been focused on therapeutic implications for stroke up to now, but it is time to consider stroke in terms of the patients’ quality of life.
Stroke causes deterioration in the quality of life as well as mental problems such as depression due to physical problems like hemiplegia where patients continue their lives with chronic disabilities while depending on others for a long time. Lee (2001) reported that patients with hemiplegia have psychological difficulties such as depression, anxiety, and decreased self-esteem as well as reduced quality of life in addition to problems of functional disorders, motor control, and activities of daily living. These patients were also found to experience distresses such as anxiety due to deterioration of activities of daily living and fear for the future (Cho et al., 2003).
Recently, concerns are shifting away from the paradigm focusing on negative effects due to disease resilience towards positive psychology focusing on the strength and resources of humans as well as promoting human growth (Seligman and Csikszentmihalyi, 2000). Resilience refers to the concept expressing the psychological ability of an individual to recover from adversity and to adapt positively (Wagniid and Young, 1993). In other words, it is the ability to convert difficult situations, adversity, stress, or pain occurring in life into experiences to overcome (Polk, 1997). Considering the result of a study which reported that resilience had a positive effect on the survival period (Oh, 2009), overall disease recovery process, and quality of life in cancer patients who have to struggle against disease for a long time (Hasse, 2004), it can be inferred that resilience through rehabilitation of patients with chronic hemiplegia will be an important factor that may restore physical functions and increase quality of life. In addition, the degree and time to recover from stroke can differ by location of occurrence, damage, and age. Therefore, it is important to start rehabilitation as soon as possible and maintain continuous treatment.
Advanced research on motor rehabilitation of patients with stroke has concentrated on functional aspects including rehabilitation for the recovery of upper limb motor functions (Choi et al., 2014), walking (Smulders et al., 2012), or rehabilitation related to balance (Hyndman et al., 2006). Investigations of the association between such functional recovery and ADL (Kim and Lee, 2013) have also been conducted. It is important to begin comprehensive rehabilitation from bedside activities, lying down, or sitting immediately after acute phase treatment in the early stage (Liepert et al., 1998; Page et al., 2002). Also, although patients attempt to return to ADL through physical and occupational therapies which are implemented in hospitals, they cannot perform the functions when they face the actual environment (Kang and Goo, 2013). Most programs are designed for patients with acute or subacute conditions, but accessible rehabilitation programs for chronic patients are not generalized. Thus, it is urgent to develop a realistic rehabilitation program.
This study, therefore, attempts to design a repeatable and universal rehabilitation program in which patients with hemiplegia can participate voluntarily in addition to physical and occupational therapy in order to increase the voluntary exercise practice rate. Also, the relationship between psychological resilience due to the implementation of self-bedside exercise and functional recovery of ADL will be evaluated in this study. The purpose of this study is to provide basic data of motor rehabilitation for those who have difficulties in moving their bodies including patients with hemiplegia as a result of aging and diseases.
MATERIALS AND METHODS
Selection of subject
The subjects of this study were patients with chronic hemiplegia who stayed more than 6 months in M rehabilitation hospital located in Incheon and consented to participate in the study. Those who were able to communicate well with a score of 25 or more in the result of Mini Mental Status Examination were selected. Out of 15 patients who consented to participate, a total of 12 subjects, excepting 3 patients who were discharged, completed the program.
Self bedside exercise program
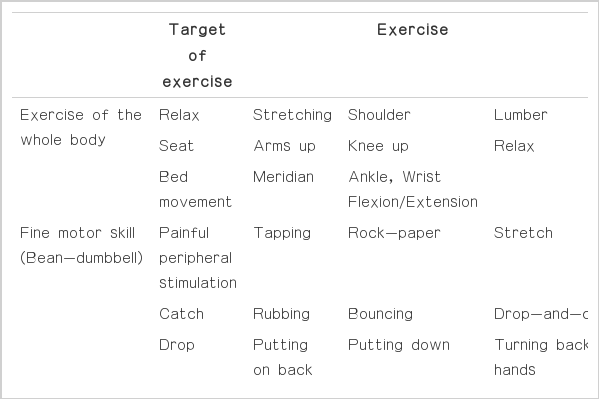
The purpose of this study was to design a voluntary, repeatable rehabilitation program that can be universalized for patients with chronic hemiplegia. The study consists of a program that can be conducted from the bedside in consideration of the degrees of various symptoms and safety of patients. This program can be divided into exercise of the whole body, fine motor skill, and motor coordination, with a total of 30 exercises in 3 stages (Table 1). The goal of the program was to perform a total of 10–13 exercises using 1 or 2 exercises in the level applicable to the patient according to each goal.
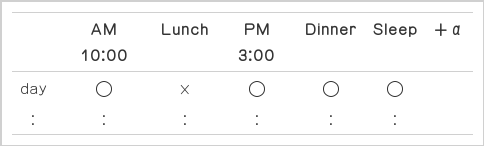
The total exercise duration was approximately 10 min, and the instructor visited once a day to correct the exercises and set goals during the experiment period (Table 2). The individual subjects were instructed to freely perform the exercise more than 5 times a day. The exercise program was conducted 5 times a week except for Saturday and Sunday for 8 weeks, and whether they performed the exercise or not was recorded in their exercise table. The implementation rate was calculated so that if a patient completed the exercise 3 times out of 5 in one day, it was then calculated as 3/5 day×100=60%.
Resilience test
For the resilience test measuring instrument, the Korean Version of the Connor-Davidson Resilience Scale, which is the translated and validated version by Baek et al. (2010) of Connor-Davidson Resilience Scale (CD-RISC) developed by Connor and Davidson in 2003 was used. This instrument was developed for adult clinical patients and measured 5 factors including tenacity, persistency/durability, optimism, support, and spirituality. In a total of 25 questions, the 5-point scale ranged from 1 point of ‘Not at all’ to 5 points of ‘Very much so’ and a high score implied a high level of resilience. When the instrument was first developed by Connor and Davidson (2003), the reliability was Cronbach’s α=0.89, and it was Cronbach’s α=0.91 in the study by Baek et al. (2010). In this study, the reliability was Cronbach’s α=0.97.
ADL assessment
Modified Barthel Index: MBI
MBI is composed of 10 items including personal hygiene, taking a bath alone, eating, using the bathroom, ascending stairs, dressing, defecating, controlling urine, walking or using a wheel-chair, and moving to a chair or bed. Each item consists of 5 steps ranging from independent conduct, minimum assistance, intermediate assistance, maximum assistance, and impossible to conduct (Jung et al., 2007).
Manual Function Test: MFT
MFT an evaluation instrument for upper limb functions developed by Tohoku University, Japan, is designed to measure the recovery upper and lower limb functions and activities of daily living of patients in a practical way. There are a total 32 composition items, including 8 items in 3 domains of upper limb exercise, holding, and finger tissue. The instrument used in this study was the one complemented and revised for Koreans by Yoo et al. (2006).
Berg Balance Scale: BBS
To evaluate balance ability of the subjects, a BBS which measures static and dynamic balance abilities was used. This instrument, developed by Berg et al. (1995), consists of 14 items of functional tasks generally performed in activities of daily living every day. 3 domains of sitting, standing, and changing posture are applied from a minimum of 0 to a maximum of 4, with a total of 56 points as full mark. This instrument was originally developed to assess elderly stroke patients, revealing sensitive measurements in recovery. This measuring instrument has high reliability and validity with r=0.99, the reliability within the inspector and r=0.98, the reliability between inspectors (Berg et al., 1995).
Data analysis
For the data collected in this study, mean and standard deviation for all measured values were calculated by using SPSS ver. 18.0. Paired t-test was conducted to test the difference before and after the self-bedside exercise program. Also, to examine the correlation between resilience and ADL, Pearson’s correlation analysis was performed. The level of significance was P<0.05.
RESULT
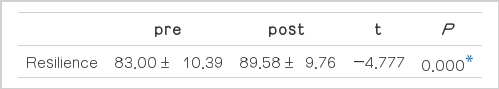
Change in resilience
The change in resilience by the 8-week self-bedside exercise program in patients with hemiplegia was an improvement from 83.00±10.39 to 89.58±9.76, showing a significant difference (t=−4.777, P<0.001) (Table 3).
Change in activities of daily living (MBI, MFT, and BBS)
The changes in ADL due to the implementation of the 8-week self-bedtime exercise of patients with hemiplegia are described in Table 4. MBI was improved from 58.33±4.83 to 61.41±5.30 and showed a significant difference (t=−6.174, P<0.001). In a comparing of MFT and upper limb motor function recovery, the affected side improved from 11.33±3.17 to 12.41±2.90 (t=−4.168, P<0.002), and BBS improved from 31.92±3.70 to 32.83±3.88 (t=−2.561, P<0.026), respectively, showing a significant difference. The unaffected side of MFT, on the other hand, was improved from 28.42±0.79 to 28.50±0.67 (t=−0.432, P<0.674), showing no significant change (Table 4).
Correlation between resilience and MBI, MFT, and BBS
ADL MBI (r=0.616, P<0.033) and upper limb motor function MFT (r=0.739, P<0.010) were found to have statistically significant positive correlations with resilience. Also, MBI and MFT (r=0.826, P<0.001) showed statistically significant positive correlations, and MBI (r=0.578, P<0.049) and MFT (r=0.732, P<0.007) had statistically significant positive correlation with BBS (Table 5).
DISCUSSION
Modern society can be said to be the aged society as well as the age of longevity with diseases. Therefore, the focus is not only on treatment of diseases but also on care and disease resilience. The roles of rehabilitation required by the modern society should not be limited only to the maximization of loss of function and reduction of dependence for ADL, but also be expanded to helping patients return and adapt to the society to improve their quality of life.
Resilience refers to the process in which an individual exerts positive adaptive ability despite experiencing serious mental shock or unfortunate incidents (Luthar et al., 2000). Most patients with stroke experience disabilities in ADL (You et al., 2014) with patterns of social maladjustment such as helplessness and depression (Karahan et al., 2014). Therefore, rehabilitation for patients with stroke should focus on comprehensive rehabilitation centered on independent ADL and psychological adjustment (Lim et al., 2009) in achieving successful rehabilitation, the improvement of resilience which promotes recovery intention along with functional rehabilitation.
In advanced studies, the average resilience for patients with colorectal cancer, hematological cancer, and breast cancer, all diseases that have high mortality in Korea similarly to stroke, were compared. The resilience of patients with colorectal cancer was 83.92±26.95 (Kim and Byeon, 2013), hematological cancer was 71.07±13.25 (Kwak and Byeon, 2013), and breast cancer was 89.27±14.95 (Ha et al., 2014), all of which are similar to the pre-resilience of patients with stroke in this study. Resilience is reported to have a positive effect on survival period (Oh, 2009) and on the overall disease recovery and quality of life in cancer patients who have to struggle against disease for a long time (Hasse, 2004). The purpose of this study was to develop a rehabilitation program that can induce voluntary movement of patients in addition to occupational and physical therapies, with a focus on the safety and persistency of patients. Indeed, the patients who experienced this program expressed that they often touched beans-dumbbell, and it was good to exercise in adequate intensity in both affected and unaffected sides. From the results of this study, the resilience score after implementing the 8-week self-bedside exercise program was significantly increased from 83.00±10.39 to 88.75±9.77, indicating that it had a positive effect on the recovery process.
The damage of upper limb function after stroke is one of the most common aftereffects, and the recovery of function in the affected side is only 30–60% in spite of patients receiving long-term treatment (Jorgensen et al., 1995). Because of this disease, asymmetric physical dependence emerges, including unbalancing of the body, impaired weight movement ability, and deficit of voluntary movement (Li et al., 2007). This affects the decrease of balancing ability when walking and negatively influences the delicate function performance of the limb (Lerox et al., 2006). Thus, ADL in patients with chronic hemiplegia is closely related to limb function and balance control ability (Hsieh et al, 2002; Hyndman et al., 2006).
From the results of this study, after implementing the 8-week self-bedside exercise, significant increases were found in MBI, BBS, and MFT in the affected side, but no significant change was found in MFT in the unaffected side. Park et al. (2011) confirmed the significant increases in MBI and BBS after implementing an exercise program in the bedside environment, while Hong (2011) reported that ADL significantly increased in the exercise group. Therefore, it can be said that their results support the effectiveness of the self-bedside exercise program conducted in this study.
Finally, in the correlation analysis between resilience and MBI, MFT, and BBS, resilience showed positive high correlations with ADL MBI (r=0.616, P<0.033) and upper limb motor function MFT (r=0.739, P<0.010). There is no advanced research related to this result, but it was noted that the implementation of the self-bedside exercise program for patients who participated in this study program reached 108.5±12.44%, and the implementation showed a statistically positive correlation with resilience (Table 6). Such results can be seen as an indication that voluntary participation, the goal of this program, was well induced. It was surmised that the increase of resilience was affected by several factors; a familiar instrument called the bean-dumbbell was used, the goal setting of simple movement enhanced confidence of movement, and voluntary participation was possible. It was also thought that the high rate of implementation played a positive role in functional recovery. In addition, MBI showed a high correlation with MFT in the affected side, and as a result of analyzing the related factors, all three domains in MFT including limb function, grasping power, and finger control were related to MBI. It was concluded that the application of fine motor skills using the bean-dumbbell had a positive effect on limb function, and that motor coordination had a positive effect on balance in this study.
The purpose of this study was to design a universal rehabilitation program in which patients with hemiplegia can participate voluntarily to increase voluntary movement in addition to physical therapy and occupational therapies. Also, this study attempted to identify the relationship between psychological resilience due to the implementation of self-bedside exercise and functional recovery of ADL. 12 patients with hemiplegia voluntarily participated in 8 weeks of self-bedside exercise 5 times a day and more than 5 days a week. Their program implementation, resilience, activities of daily living (MBI), upper limb motor functions (MFT), and balance ability (BBS) were analyzed and compared before and after the program.
Compared to before implementing the program, significant increases were found in resilience, MBI, BBS, and MFT in the affected side after the implementation, and the resilience scores showed statistically positive correlation in MBI and MFT. Also, the change in resilience before and after the program implementation showed a statistically positive correlation.
Therefore, it can be concluded that the self-bedside exercise developed in this study had a positive effect on voluntary participation in exercise as well as resilience and ADL. However, many studies which complement the psychological aspects of hemiparetic patients with stroke are still needed, and the studies of movement for patients or the elderly including patients with stroke who have to stay in hospital or in bed for a long period of time must be continued.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.