Exonic polymorphism (rs315952, Ser133Ser) of interleukin 1 receptor antagonist (IL1RN) is related to overweigh/obese with hypertension
Article information
Abstract
Recent studies demonstrated that interleukin 1 receptor antagonist (IL-1RN) plays an important role in metabolic effects. To investigate whether IL1RN polymorphisms are associated with obesity, two single nucleotide polymorphisms (SNPs) of the IL1RN gene [rs4251961 (-828, T> C) and rs315952 (Ser133Ser)] were analyzed in 122 overweigh/obese and 123 control subjects. Overweigh/obese subjects were classified according to body mass index (BMI). SNPStats was used to obtain odds ratios (ORs), 95% confidence intervals (CIs), and P values. Multiple logistic regression models (codominant1, codominant2, dominant, recessive, and log-additive) were conducted to analyze the genetic data. Synonymous SNP (rs315952) of the IL1RN gene was associated with overweigh/obese with hypertension (OR= 4.98, 95% CI= 1.74–14.19, P = 0.003 in codominant 1 model and OR= 3.98, 95% CI= 1.48–10.74, P= 0.0029 in dominant model). However, another SNP (rs4151961) did not show association with overweigh/obese or overweigh/obese with hypertension. These results suggest that exonic SNP of IL1RN (rs 315952, Ser133Ser) may be contributed to overweigh/obese with hyper-tension.
INTRODUCTION
Exercise rehabilitation provides benefit to assisting in the physical state including blood pressure, blood sugar, and vessel elasticity in obesity (Lee et al., 2013). Although exercise rehabilitation is effective in obesity patients, there are various differences among obesity patients. Hence, it is important to find clinical characters of obesity patients in order to do exercise rehabilitation.
Obesity is the primary metabolic disorder and is well known to play a key role in the development of a number of metabolic abnormalities (Pi-Sunyer, 2002). Obesity increases the susceptibility of many diseases, such as type 2 diabetes mellitus, hypertension, and various cancers (Foss and Dyrstad, 2011). Obesity is characterized by an increased adipose tissue mass with large size and mature adipocytes. The obesity results in an imbalance between energy in-take and energy expenditure. Environmental, behavioral, and genetic factors have been known to contribute to the etiology of obesity (Foss and Dyrstad, 2011).
Interleukin 1 (IL1) is a regulator on inflammation and energy homeostasis. Previous studies investigated that the IL1 system was contributed to metabolism (Erion et al., 2014; Khalkhal et al., 2012). Interleukin 1 receptor antagonist (IL1RN) is included in the IL1 system. IL1RN is an acute-phase protein. IL1RN has an anti-inflammatory function by blocking the receptor for IL1A and IL1B without exerting any biological effect (Juge-Aubry and Meier, 2002).
Previous study revealed that IL1RN is associated with obesity (Somm et al., 2005). IL1RN showed high level in the serum of obese patients and overexpressed in white adipose tissue. Somm et al. (2005) reported that IL1RN knockout mice get leanness and obesity resistance. It indicated that IL1RN is an important regulator of adipogenesis, food intake, and energy expenditure in obesity. In this study, we investigated whether polymorphisms of the IL-1RN gene are associated with the development of obesity.
MATERIALS AND METHODS
Study subjects
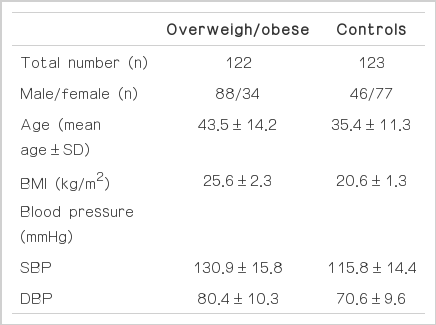
Table 1 shows the clinical characteristics of subjects in this study. Subjects were recruited among participants who examined a general health check-up program. Each subject was calculated body mass index (BMI), systolic blood pressure (SBP), and diastolic blood pressure (DBP). BMI was also used by dividing the subject’s mass by the square of height (kg/m2). According to the classification of Korean Society for the Study of Obesity (underweight, BMI<18; normal, BMI 18 to<23; moderately obese, BMI 23 to<25; obesity I, BMI 25 to<30; obesity II, BMI≥30), subjects were divided into two subgroups, the overweigh/obese group (BMI≥23, n=122) and the normal group (18<BMI<23, n=123). And overweigh/obese subjects also divided into two subgroups, the overweigh/obese with hypertension group (>130 mmHg in SBP/>85 mmHg in DBP, n=40) and the overweigh/obese with non-hypertension group (<130 mmHg in SBP/<85 mmHg in DBP, n=98). The subjects with severe diseases, such as stroke, diabetic mellitus, and cancers were excluded in this study. Ethical approval of this study was obtained from the ethics review committee of Medical Research Institute, School of Medicine, Kyung Hee University, Seoul, Korea.
SNP selection and genotyping
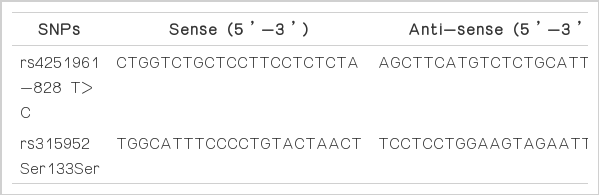
We selected two SNPs in the IL1RN gene: [rs4251961 (-828, T>C) and rs315952 (Ser133Ser)]. They were searched from the SNP database in NCBI (http://www.ncbi.nlm.nih.gov/SNP, db141), and reviewed to select in the exon area and the promoter area. Peripheral blood of all subjects were collected in EDTA blood tube, stored in −20°C freezer before the extraction of genomic DNA. Genomic DNA was extracted with Roche DNA extraction kit (Indianapolis, IN, USA). Polymerase chain reactions (PCRs) of the SNPs were conducted using the following primers in the Table 2 to amplify target sequences including these SNPs [rs4251961 (-828, T>C) and rs315952 (Ser133Ser)]. PCR condition was 38 cycles at 94°C for 30 sec, 58°C for 30 sec, and 72°C for 30 sec. PCR products were identified with 1.8% agarose gel by electrophoresis. Each PCR product was analyzed by direct sequencing in order to obtain the genotype of each SNP. Direct sequencing, sequence sorting, and genetic data were performed by ABI PRISM 3730XL analyzer (PE Applied Biosystems, Foster City, CA, USA) and SeqManII software (DNASTAR, Madison, WI, USA).
Statistical analysis
Hardy-Weinberg equilibrium of each SNP was examined in SNPstats. SNPStats (http://bioinfo.iconcologia.net/index.php?-module=Snpstats) and SPSS 18.0 (SPSS Inc., Chicago, IL, USA) also were used to obtain odds ratios (ORs), 95% confidence intervals (CIs), and P values. Multiple logistic regression models were applied in the analysis of genotypes (Kim et al., 2014; Yang, 2013). The haplotype analysis in two SNPs of the IL1RN gene was analyzed with Haploview 4.2 software (Daly Lab, Cambridge, MA, USA). In the statistical analysis, P<0.05 was considered significant association.
RESULTS
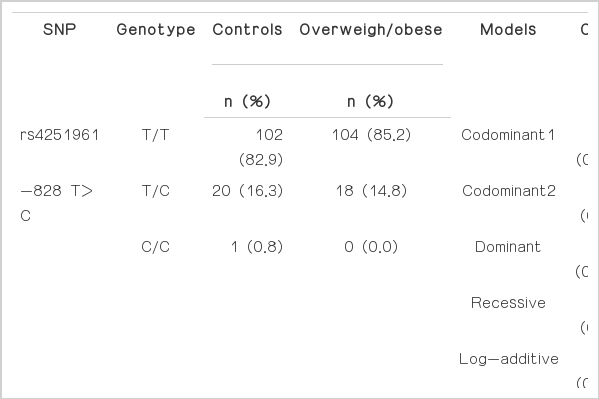
Table 3 shows the genotype and allele frequencies of two SNPs (rs4251961 and rs315952) between the normal group and the overweigh/obese group. The risk of obesity was performed by logistic regression analysis. Genotype distributions of two SNPs in this study were in Hardy-Weinberg equilibrium in control subjects (rs4251961, P=1.00; rs315952, P=0.35, data not shown).
Frequencies of rs4251961 SNP genotype of the IL1RN gene in the normal group and the overweigh/obese group were 82.9%: 16.3%:0.8% and 85.2%:14.8%:0.0% (T/T genotype:T/C genotype:C/C genotype). Frequencies of rs4251961 SNP in the normal group and the overweigh/obese group were 91.1%:8.9% and 92.6%:7.4% (T allele:C allele).
Frequencies of rs315952 SNP genotype of the IL1RN gene in the normal group and the overweigh/obese group were 33.3%: 52.9%:13.8% and 32.0%:50.8%:17.2% (C/C genotype:C/T genotype:T/T genotype). Frequencies of rs315952 SNP in the normal group and the overweigh/obese group were 59.8%:40.2% and 57.4%:42.6% (C allele:T allele). There were differences of the genotype and allele frequencies in the normal group and the over-weigh/obese group. However, the differences did not show any significant association with obesity (P>0.05).
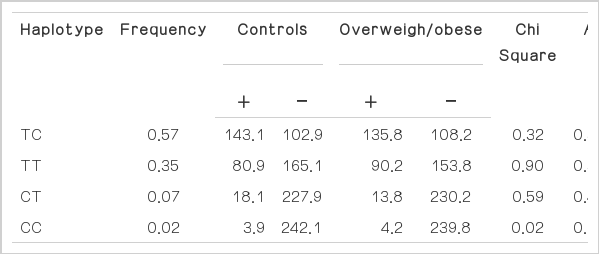
Two SNPs (rs4251961 and rs315952) of the IL1RN gene were analyzed for haplotype analysis using Haploview 4.2. There were four haplotypes (haplotype TC, frequency=0.57; haplotype TT, frequency=0.35; haplotype CT, frequency=0.07; haplotype CC, frequency=0.02) (Table 4). The difference between the normal group and the overweigh/obese group also did not show any association with obesity (P>0.05).
In clinical analysis, the overweigh/obese subjects were divided into two subgroup according to hypertension. Frequencies of rs315952 SNP genotype of the IL1RN gene in the overweigh/ obese with the non-hypertension group and the overweigh/obese with hypertension group were 36.7%:45.9%:17.4% and 15.0%: 67.5%:17.5% (C/C genotype:C/T genotype:T/T genotype). In the genotype distribution analysis, the difference of genotype frequency of rs315952 SNP showed significant association with hypertension [OR=4.98, 95% CI=1.74–14.19, P=0.003 in codominant 1 model (C/C genotype versus C/T genotype) and OR=3.98, 95% CI=1.48–10.74, P=0.0029 in dominant model (C/C genotype versus C/T genotype+T/T genotype), Table 5]. Another rs4251961 SNP was not associated with hypertension. The results suggested that rs315952 SNP was associated with overweigh/obese with hypertension.
DISCUSSION
In this study, we investigated the relationship between two SNPs (rs4251961 and rs315952) of IL1RN and obesity. IL1RN has biological function in human body. The IL1 system included several components, such as two agonists, IL1A and IL1A. The biological effects are exerted via the interleukin 1 receptor, type I (IL1R1). The binding of IL1 to IL1RI can be inhibited by the endogenous receptor antagonist IL1RN. The balance between IL1 and IL1RN plays an important role in the regulation of immune function (Arend, 2002; Dinarello, 1991; Strandberg et al., 2006). Previous study suggested that IL1 system was contributed to body fat accumulation in animal experiment. Matsuki et al. (2003) showed that increased IL1 activity due to IL1RN knockout results in resistance to obesity.
There were several genetic researches regarding the relationship between IL1RN polymorphisms and obesity (Andersson et al., 2009; Um et al., 2006). Um et al. (2004) investigated that 86 bp tandem repeat (VNTR) in the intron 2 of IL1RN was associated with obesity. The genotype and allele distributions of VNTR in IL1RN did not show association with obesity. However, Andersson et al. (2009) reported that rs4252041 SNP (3’-untranslated region, UTR) was associated with the primary outcome total fat mass and regional fat mass. We also investigated the relationship between IL1RN polymorphism (rs315952, Ser133Ser) and obesity and found significant association in obesity patients with hypertension. The rs315952 SNP of the IL1RN gene was investigated in various diseases including metabolic syndrome, systemic lupus erythematosus, ankylosing spondylitis, and osteoarthritis (Meyer et al., 2014; Oh et al., 2010; Tahmasebi et al., 2013; Wu et al., 2013). However, the 86 bp VNTR in the intron 2 of IL-1RN was not associated with essential hypertension in a Pakistani Pathan population (Khawaja et al., 2008).
In conclusion, we investigated the relationship between two SNPs (rs4251961 and rs315952) and obesity. One synonymous SNP (rs315952, Ser133Ser) of the IL1RN gene was associated with overweight/obesity with hypertension. The result suggested that IL1RN may be contributed to the development of obesity with hypertension. However, another cohort and functional studies will be needed to confirm this result in further study.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.