AbstractThis study aimed to examine the effects of exercise interventions developed over the past 10 years to prevent falls among older adults. Cochrane, PubMed, and Embase databases were systematically searched on November 3, 2022, using the following keywords: “elderly” or “aged” and “fall prevention exercise” and “randomized controlled trial.” A total of 918 articles were retrieved, and finally, 18 studies were included in the meta-analysis. main conclusions were as follows: fall prevention exercises showed moderately positive effects on balance, gait, mobility, physical function, lower limb power, and strength, but low effects on proprioception, vision, and reaction speed. The effect sizes were highest when the intervention period was 1–24 weeks, time was 31–60 min, and frequency was thrice per week. Place of intervention (home, community, laboratory) and age (>75 years, <75 years) showed similarly moderate effect sizes. A combined program that includes balance, co-ordination, and resistance exercises is appropriate to improve fall-related fitness and fall efficacy in community-dwelling older individuals.
INTRODUCTIONFall is a serious health problem for older individuals because it is difficult to recover from physical damage or functional disability after a fall, the degree of injury is more severe, and may even cause death (Rubenstein, 2006). When older adults experience a fall, independent activities become difficult owing to their fear of falling, and their level of physical activity decreases. This leads to a vicious cycle that increases the risk of falling (Jefferis et al., 2014). In recent years, the risk of falls has emerged as an important healthcare problem in older adults because when the number of fall increases, medical costs increase. The importance of intervention programs for preventing falls for older individuals has been recognized, and various types of programs have been implemented. Studies on this are conducted widely because earlier, it was believed that falls were unavoidable as they occurred without a specific cause; however, recently, the perception has changed that falls are preventable by removing or alleviating their risk factors (Rubenstein and Josephson, 2006).
Various intrinsic and extrinsic factors affect the risk of fall, and multiple fall prevention programs have been designed to reduce this risk. Several systematic literature reviews related to fall prevention programs that support the effectiveness of multifactorial interventions in preventing falls among older adults have been published. These interventions included exercise, education, environmental modification, medication, mobility aids, vision, and psychological management (Lee and Yu, 2020). Chang et al. (2004) reported three findings through a meta-analysis: (a) multifactorial interventions significantly reduced fall rates in both high-risk and healthy groups compared with usual care; (b) exercise and environmental modifications are the key components of effective multifactorial fall prevention interventions; and (c) key intervention components focusing on exercise and environmental modification are recommended among the multifactorial fall prevention interventions. However, exercise is reported as a representative factor in lowering the risk of falls in older adults in the meta-analysis; in contrast, there are few studies that reviewed the literature only for exercise programs. In addition, exercise guidance is provided to older individuals for fall prevention, and there are studies that statistically reviewed whether such exercises have a positive effect on the improvement of fall-related physical fitness and physical function. Recently, many exercise programs for preventing falls have been developed, and it is important to review their effects. The novelty of this study is to comprehensively review the existing literature and suggest of the type and the way (frequency, place, time) of exercise to increase fall efficacy and fall-related physical fitness in the older adults.
Therefore, the purpose of this study was to conduct a meta-analysis of fall prevention exercise interventions developed over the past 10 years, and to find out which exercise interventions are effective for fall-related physical fitness and fall efficacy in community-dwelling older individuals.
MATERIALS AND METHODSReporting standardsThe review was conducted in accordance with the PRISMA (preferred reporting items for systematic reviews and meta-analysis) guidelines (Moher et al., 2009) and the recommendations of the Cochrane collaboration (Higgins and Thompson, 2002).
Search strategySearch criteria were established to systematically select articles based on the population intervention comparison outcomes framework. First, study participants were community-dwelling older individuals aged over 60 years (Population). Second, the intervention method was limited to fall prevention exercises (Intervention). Third, research with an experimental design in the form of a comparison of results through pre- and post-tests were selected (Comparison). Fourth, parameters related to physical fitness and fall efficacy were selected as a dependent variable of the intervention (Outcome). Studies presenting specific statistical values for effect size (ES) calculation were selected. To identify the literature, Cochrane, Embase, and PubMed databases were search on November 3, 2022, using the following keywords: “elderly” or “aged” and “fall prevention exercise” and “randomized controlled trial (RCT).” A total of 918 papers were retrieved. Among the extracted papers, 283 duplicates and 396 systematic reviews, reports without text, and reports published before 2012 were removed. Next, 125 irrelevant articles, 56 unclear, and 40 in which the outcomes or contents were not related to the purpose of this study were removed. Finally, 18 studies were analyzed (Fig. 1).
Data extraction and codingTwo independent researchers with doctoral degrees in health science-related fields extracted the following data from the selected RCTs: participant details (sample size, age, and sex), intervention characteristics (methods, frequency, etc.), outcomes of interest, and results. Coding was conducted after writing a book to analyze the characteristics of the literature. Coding items were author (year of publication), participants, number of cases in the group, age, intervention period, and outcome variables (statistical value for each physical fitness variable). Outcomes were classified in two steps. In step 1, the parameters were divided into factors and were categorized as follows: balance, mobility, cognition, depression, fall efficacy scale (FES), gait, power reaction time, range of motion (ROM), strength, vision, and proprioception. In step 2, parameters with similar results were categorized as same factors to minimize the amount of information lost when analyzing each parameter.
Analysis methodsThe coded data were analyzed using Comprehensive Meta-Analysis 3.0. First, the effect of each outcome parameter was calculated as Cohen d. ES was categorized as follows: <0.40, small; 0.40–0.70, moderate; >0.70, large. Second, Q and I2 were calculated to verify the heterogeneity of the ES. Cochran Q test is a traditional test for heterogeneity in meta-analyses. It is based on a chi-squared distribution; large produces a probability that exhibits greater variability across studies, rather than within participants of a study. If the P-value for Cochran Q was <0.1, it was possible to determine whether there was heterogeneity in the ES. Mathematically, I2 is expressed as I2=τ2/(σ2+τ2), where τ2 denotes the between-trial heterogeneity, σ2 denotes some common sampling error across trials, and σ2+τ2 is the total variation in the meta-analysis. The heterogeneity of I2 was interpreted as follows: 0%–25%, low; 25%–49%, medium; 50%–74%, high; and 75%–100%, quite high (Higgins and Thompson, 2002). Fixed-effects or random-effects model was used if homogeneity or heterogeneity was determined, respectively. A quality assessment in this study was also independently conducted by two researchers using the Cochrane risk of bias for RCTs, which assessed selection, allocation, performance, detection, attrition, and reporting biases; the scores were categorized as low-risk, unclear, and high-risk. Finally, publication bias of the results was verified using Funnel plot and Egger regression analysis.
RESULTSHomogeneity test and total ESThe results of the homogeneity test related to the effect of the fall intervention exercises on the parameters are shown in Table 1. The statistical significance of the Q value was less than 0.000, and I2 was 79.98; therefore, the heterogeneity was greater than moderate. Consequently, it was assumed that the articles included in this study were not homogeneous, as analyzed using the random-effects model. According to Cohen d coefficient, the ES was moderate (0.54).
Risk of biasA summary of the quality assessment results is presented in Fig. 2. The quality assessment revealed that three studies had a high risk of performance bias, and that several studies reported unclear blinding of participants and personnel and selective reporting.
ES for each physical fitness factor and FES
Table 2 shows the effect of fall prevention exercises on FES and physical fitness, and the results of the subgroup analysis of participants’ age, intervention period, frequency, time, and place. First, the ES of the FES, an index representing fall efficacy, was 0.64, which was statistically significant. Regarding physical fitness variables, mobility (ES=0.74) and gait variables (ES=0.66) showed high ES of 0.7; balance (ES=0.58), center of pressure (ES=0.61), and physical function (ES=0.61) had moderate ES; and lower limb muscle power (ES=0.65) and muscle strength (ES=0.68) had high ES. Upper limb strength (ES=0.52) and upper limb power (ES= 0.24) showed medium to small effects. Awareness of mobility (ES= 0.45) and physical function (ES=0.38) showed moderate effects. In contrast, cognition (ES=0.27), reaction time (ES=0.29), ROM (ES=0.34), depression (ES=0.24), vision (ES=0.23), and proprioception (ES=0.30) had small effects.
ES for each age, intervention period, frequency, and time parameterAs a result of the subgroup analysis by classifying the age of participants in the intervention program based on the age of 75 years, both groups of <75 and ≥75 years showed moderate ES of 0.6 (ES=0.57, 0.59). According to intervention period, the groups with 1–12 and 13–24 weeks’ period showed moderate ES of 0.6 (ES=0.59, 0.55); however, the group with 25–48 weeks showed a small ES of 0.3. For the intervention time, the ES of 31–60 min was the largest (0.69), followed by 61–90 min (0.47), and ≤30 min (0.28). Regarding the frequency of interventions, the ES of thrice per week was the largest (0.69). Subgroup analysis by intervention location showed that community (ES=0.56), laboratory (ES=0.53), and home (ES=0.56) had moderate ESs. Characteristics of included studies were shown in the Table 3.
Publication bias assessment
Fig. 3 shows the results of Funnel plot and Egger regression analyses of the publication bias of the meta-analysis. Egger’s regression intercept significance test was not statistically significant (intercept=−0.63, standard error=1.04; P=0.55). Therefore, there was no significant publication bias.
DISCUSSIONFall risk factors can be divided into two categories: (a) extrinsic such as lighting intensity, height, slope of indoor and outdoor floors, aspects related to the surrounding environment such as bathroom floors; and (b) intrinsic such as physical factors of muscle weakness, gait disorders, and drug intake (Hill-Westmoreland et al., 2002). Falls occur or recur because of a lack of mobility or activity due to aging, such as lower- and upper limb muscle weakness, balance and gait disorders, visual acuity loss, and sensory deterioration. If these risk factors are reduced in advance, falls can be prevented. This meta-analysis examined the effects of fall prevention exercise programs conducted over the last 10 years on fall-related physical fitness and their fall efficacy.
It was found that exercise interventions had positive effects on FES. When older adults experience a fall, their physical activity decreases because of their fear of falling, making it difficult for them to live independently. In contrast, people who are capable of physical activity and have a high level of fall-related physical fitness have high “fall efficacy,” which means that they are not afraid of falling.
In older individuals who participated in the fall prevention exercise programs, the amount of physical activity and level of fall-}related physical fitness increased by actively performing the exercises, leading to an increase in fall efficacy. People with high fall efficacy experienced fewer falls than others. However, Merom et al. (2016) reported that because the participants gained confidence due to the intervention, their exposure to walking increased and, consequently, they experienced more falls. In other words, regular exercise reduces the risk of falling, but frequent physical activity can increase the risk of falls (Hwang et al., 2016). It is necessary to review follow-up studies on the long-term effects of increased physical activity through various interventions on fall risk.
Overall, balance, gait, mobility, physical function, lower limb power, and strength had moderate or high positive effects; however, proprioception, vision, and reaction speed had no significant effects. A meta-analysis of various fall prevention exercise programs showed an overall moderate ES of 0.54 (P<0.05). Various intervention programs have been implemented; therefore, integrating intervention programs into a few factors is challenging. Among them, the intervention program which applied an integrated exercise centered on balance, coordination, and resistance exercises had a significant positive effect on fall-related physical fitness (ES: combined exercise, 0.76; visual feedback of movement performance, 0.66; task-oriented training, 1.04; motor imagery training+task- oriented training, 1.31; proprioceptive neuromuscular facilitation, 0.68; resistance exercise, 0.91; and fall prevention exercise based on the Otago program, 1.12; Wii, 0.79). In contrast, the impact of exercise intervention programs including cognition and dance on fall-related physical fitness was not significant (ES: dual-task training, 0.36; cognitive training, 0.22; social dancing, 0.23; trunk motion visual feedback, 0.09). However, the number of interventions that included cognitive function or dance in this study was small, and most of the physical fitness items related to falls were related to balance and lower extremity muscle strength; therefore, the direct ES may be small. Many studies have reported that cognitive function significantly influences falls (Chua et al., 2019).
Falls during walking are the primary cause of accidental kinematic injuries in older individuals (Zhuang et al., 2014). Voukelatos et al. (2015) reported that a walking program delivered through mailed printed materials and phone calls did not reduce falls in older people but increased their walking behavior and physical activity levels. Simple walking can help increase physical activity; however, a specific exercise program needs to be prepared to prevent falls. According to Mesquita et al. (2015) exercises for fall prevention should provide a moderate or high challenge to balance. Moreover, this study found that a combined exercise centered on balance, resistance, and coordination was effective in improving fall-related physical fitness. Strength gains and balance improvements were associated with positive changes in spatiotemporal measures and joint kinematics, and participants who could generate more muscle force to achieve a quicker push-off speed during the final instants of the stance phase were also able to move their center of gravity further away from their base of support (Zhuang et al., 2014).
The ES were highest when the intervention periods were 1–12 weeks and 13–24 weeks, intervention time was 31–60 min, and frequency was thrice per week. Even in the same older individual, physical function, presence or absence of diseases, physical fitness level, and fall risk level are different, and the necessary conditions or programs should differ according to the characteristics of the group. Social dance programs and Tai Chi are unsuitable for seniors at a high risk of falling (Merom et al., 2016). Several exercise interventions delivered to high-risk groups have also been reported to cause excessive falls in the intervention group (Ebrahim et al., 1997; Merom et al., 2016; Sherrington et al., 2014). In other words, the results of this subgroup analysis correspond to community-dwelling older population, and individualized exercise programs should be prepared for those who are frail or have specific diseases.
Place of intervention and age showed similar moderate ES. In other words, there was a similar positive effect regardless of the place of intervention in the community, home, or laboratory and age (under or over 75 years) in community-dwelling older people. The development of a sustainable, engaging, and motivating program that can prevent falls in the long-term is important, although the implementation of a temporary fall prevention program is also significant. To date, most exercise intervention programs have been community-centered, and it is clear that they are effective in preventing falls. However, the importance of home-based exercise rather than community-based ones has recently been emphasized owing to the coronavirus disease 2019 pandemic. Indeed, Schoene et al. (2013) reported that home-based exercise is effective in reducing falls. Evidence suggests that training at home increases the long-term adherence of older adults to physical activity (Schoene et al., 2013). Considering fall prevention from a motivational and long-term perspective, it is necessary to develop a program that appropriately combines the community and home.
CONCLUSIONThis meta-analysis examined the effects of a fall prevention exercise program conducted over the last 10 years on fall-related fitness and their efficacy. Various exercise programs had moderate-to-positive effects on physical fitness (overall ES=0.54). The exercise interventions had a positive effect on FES. Overall, the programs had moderate or higher positive effects on balance, gait, mobility, physical function, lower limb power, and strength, but no significant effect on proprioception, vision, and reaction speed. The ES were highest when the intervention period was 1–12 weeks and 13–24 weeks, the time was 31–60 min, and the frequency was thrice a week. Place of intervention (home, community, laboratory) and age (over or under 75 years) showed similar moderate ES. A program that combines balance, coordination, and resistance exercises is appropriate for improving fall-related fitness and fall efficacy. In addition, fall prevention exercise programs should be developed according to the physical function, physical fitness, and fall risk of older adults. In the future, it will be necessary to examine how these fall prevention programs affect fall risk in the long-term through follow-up studies.
ACKNOWLEDGMENTSThis research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2022-0136).
REFERENCESAnson E, Ma L, Meetam T, Thompson E, Rathore R, Dean V, Jeka J. Trunk motion visual feedback during walking improves dynamic balance in older adults: assessor blinded randomized controlled trial. Gait Posture. 2018;62:342–348.
Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, Maglione M, Suttorp MJ, Roth EA, Shekelle PG. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ. 2004;328:680
Chua CHM, Jiang Y, Lim S, Wu VX, Wang W. Effectiveness of cognitive behaviour therapy-based multicomponent interventions on fear of falling among community-dwelling older adults: a systematic review and meta-analysis. J Adv Nurs. 2019;75:3299–3315.
Ebrahim S, Thompson PW, Baskaran V, Evans K. Randomized placebo-controlled trial of brisk walking in the prevention of postmenopausal osteoporosis. Age Ageing. 1997;26:253–260.
Eggenberger P, Theill N, Holenstein S, Schumacher V, de Bruin ED. Multicomponent physical exercise with simultaneous cognitive training to enhance dual-task walking of older adults: a secondary analysis of a 6-month randomized controlled trial with 1-year follow-up. Clin Interv Aging. 2015;10:1711–1732.
Hill-Westmoreland EE, Soeken K, Spellbring AM. A meta-analysis of fall prevention programs for the elderly: how effective are they? Nurs Res. 2002;51:1–8.
Hwang HF, Chen SJ, Lee-Hsieh J, Chien DK, Chen CY, Lin MR. Effects of home-based Tai Chi and lower extremity training and self-practice on falls and functional outcomes in older fallers from the emergency department-a randomized controlled trial. J Am Geriatr Soc. 2016;64:518–525.
Jefferis BJ, Iliffe S, Kendrick D, Kerse N, Trost S, Lennon LT, Ash S, Sartini C, Morris RW, Wannamethee SG, Whincup PH. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. 2014;14:114
Kwok BC, Pua YH. Effects of WiiActive exercises on fear of falling and functional outcomes in community-dwelling older adults: a randomised control trial. Age Ageing. 2016;45:621–627.
Lee SH, Yu S. Effectiveness of multifactorial interventions in preventing falls among older adults in the community: a systematic review and meta-analysis. Int J Nurs Stud. 2020;106:103564
Li F, Harmer P, Fitzgerald K, Eckstrom E, Akers L, Chou LS, Pidgeon D, Voit J, Winters-Stone K. Effectiveness of a therapeutic Tai Ji Quan intervention vs a multimodal exercise intervention to prevent falls among older adults at high risk of falling: a randomized clinical trial. JAMA Intern Med. 2018;178:1301–1310.
Lytras D, Sykaras E, Iakovidis P, Komisopoulos C, Chasapis G, Mouratidou C. Effects of a modified Otago exercise program delivered through outpatient physical therapy to community-dwelling older adult fallers in Greece during the COVID-19 pandemic: a controlled, randomized, multicenter trial. Eur Geriatr Med. 2022;13:893–906.
Marques EA, Figueiredo P, Harris TB, Wanderley FA, Carvalho J. Are resistance and aerobic exercise training equally effective at improving knee muscle strength and balance in older women? Arch Gerontol Geriatr. 2017;68:106–112.
Merom D, Mathieu E, Cerin E, Morton RL, Simpson JM, Rissel C, Anstey KJ, Sherrington C, Lord SR, Cumming RG. Social dancing and incidence of falls in older adults: a cluster randomised controlled trial. PLoS Med. 2016;13:e1002112
Mesquita LS, de Carvalho FT, Freire LS, Neto OP, Zângaro RA. Effects of two exercise protocols on postural balance of elderly women: a randomized controlled trial. BMC Geriatr. 2015;15:61
Moher D, Liberati A, Tetzlaff J, Altman DG. Reprint--preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–880.
Oh DS, Choi JD. Effects of motor imagery training on balance and gait in older adults: a randomized controlled pilot study. Int J Environ Res Public Health. 2021;18:650
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, McKenzie JE. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160
Reed-Jones RJ, Dorgo S, Hitchings MK, Bader JO. Vision and agility training in community dwelling older adults: incorporating visual training into programs for fall prevention. Gait Posture. 2012;35:585–589.
Rosado H, Bravo J, Raimundo A, Carvalho J, Marmeleira J, Pereira C. Effects of two 24-week multimodal exercise programs on reaction time, mobility, and dual-task performance in community-dwelling older adults at risk of falling: a randomized controlled trial. BMC Public Health. 2021;21:Suppl 2. 408
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35:Suppl 2. ii37–ii41.
Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am. 2006;90:807–824.
Schoene D, Lord SR, Delbaere K, Severino C, Davies TA, Smith ST. A randomized controlled pilot study of home-based step training in older people using videogame technology. PLoS One. 2013;8:e57734
Schwenk M, Grewal GS, Honarvar B, Schwenk S, Mohler J, Khalsa DS, Najafi B. Interactive balance training integrating sensor-based visual feedback of movement performance: a pilot study in older adults. J Neuroeng Rehabil. 2014;11:164
Sherrington C, Lord SR, Vogler CM, Close JC, Howard K, Dean CM, Heller GZ, Clemson L, O’Rourke SD, Ramsay E, Barraclough E, Herbert RD, Cumming R. A post-hospital home exercise program improved mobility but increased falls in older people: a randomised controlled trial. PLoS One. 2014;9:e104412
Smith-Ray RL, Makowski-Woidan B, Hughes SL. A randomized trial to measure the impact of a community-based cognitive training intervention on balance and gait in cognitively intact Black older adults. Health Educ Behav. 2014;41:1 Suppl. 62s–69s.
Tiedemann A, O’Rourke S, Sesto R, Sherrington C. A 12-week Iyengar yoga program improved balance and mobility in older community-dwelling people: a pilot randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2013;68:1068–1075.
Voukelatos A, Merom D, Sherrington C, Rissel C, Cumming RG, Lord SR. The impact of a home-based walking programme on falls in older people: the Easy Steps randomised controlled trial. Age Ageing. 2015;44:377–383.
Fig. 2Risk of bias summary and risk of bias graphy: a summary of the results of quality assessement. 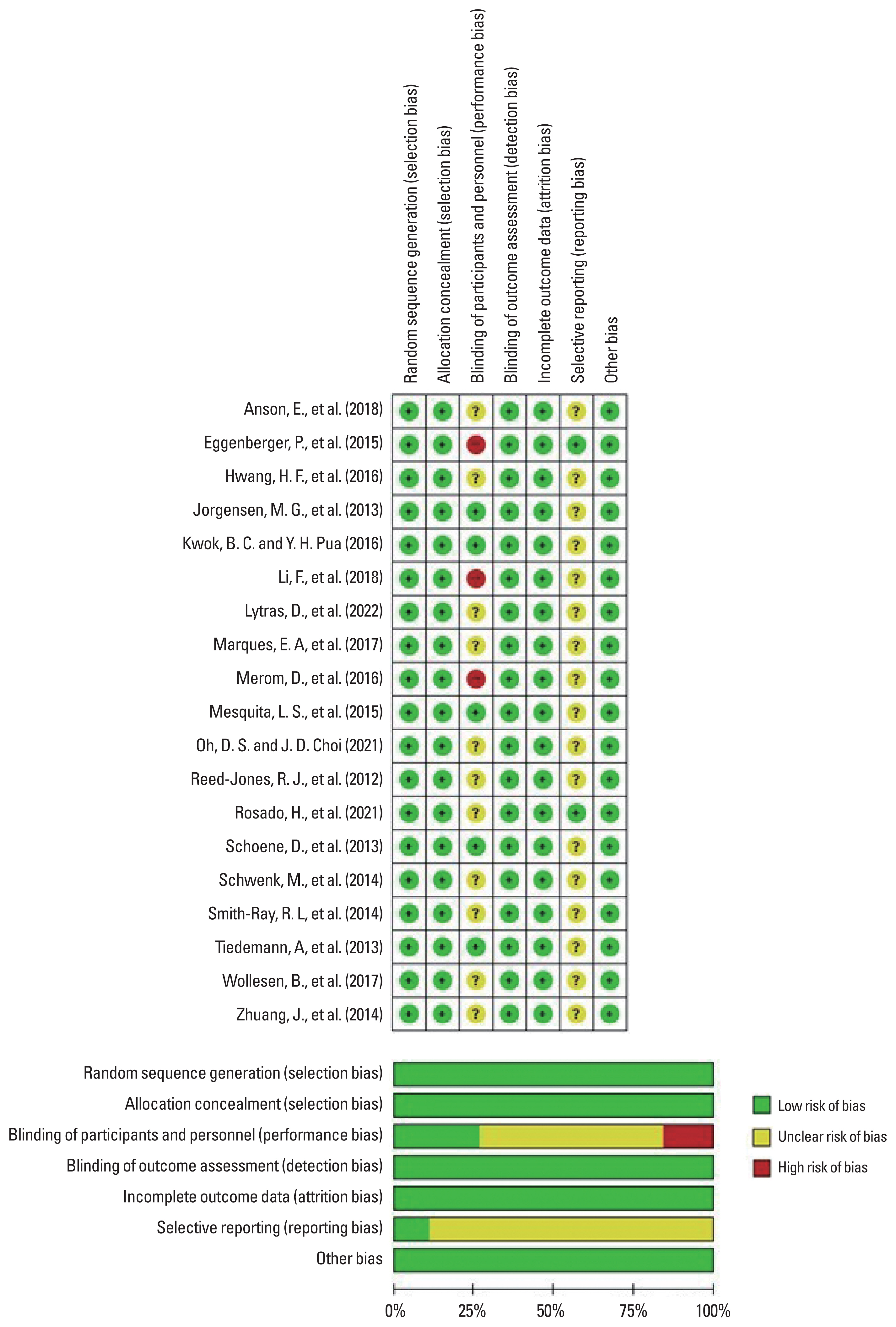
Table 1Meta-analysis results – overall effect sizes and heterogeneity Table 2Subgroup analysis results - effect sizes and heterogeneity Table 3Characteristics of included studies
VFB, trunk motion visual feedback; TCC, Tai Chi Chuan; OEP, Otago exercise program; ACSM, American College of Sports Medicine; PNF, poprioceptive neuromuscular facilitation; MITG, motor imagery training; TOTG, task-oriented training; WBV, whole-body vibration program; RT, resistance training; DT, dual task; EF, executive function; DDR, exergame dance revolution. |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||