INTRODUCTION
Using water as a modality can have a synergistic affect when combined with a land-based program, both theoretically and practically. This approach allows for a whole-body focus, with special attention on activating and relearning proper biomechanics in injured areas. Additionally, water as a modality can both strengthen and facilitate the whole body; water’s unique properties can reduce impact of exercise on joints, increase pain-free movement, improve microcirculation, and help increase muscle tone through natural resistance (Becker, 2009).
This article discusses principles and research regarding the benefits of water as an exercise and therapeutic medium, as well as the value of combined water and land therapy programs, which can help clients better realize and expand their goals of rehabilitation, conditioning, and training. In fact, an optimal program would not incorporate land without water, and vice versa. To provide one example of a potential framework, described below are the basic principles and components of the Burdenko Method (TBM), a system developed over four decades ago which has been studied in research literature and has combined exercise in both water and land to effectively treat clients in a variety of clinical settings (Burdenko et al., 2017).
WATER THERAPY: HISTORY AND PRINCIPLES
Water is ubiquitous - it is an essential substance for humanity as we are all born in water. Jacques Cousteau, French Naval officer, marine conservationist, and researcher who codeveloped the Aqua-Lung, once astutely stated, “We forget that the water cycle and the life cycle are one.” This idea is encapsulated by the fact that the first nine months of life are spent floating in a gravity-free water-based medium, through which we develop our sense of awareness and ability to move. Amniotic fluid acts as a transit system that facilitates exchange of critical solids and gases while also detoxifying and nourishing. As such, it should be no surprise that water can impart healing properties during all stages of life. Water creates a unique environment inherently accommodating to exercise, because of its 3-fold power of providing support through buoyancy, physiologic assistance through hydrostatic pressure, and controlled pain-free progression through resistance (Becker, 2009).
After life begins in water from birth, significant energy is spent balancing the pull of gravity, the effects of which accumulate as we mature and age, particularly in our musculoskeletal and connective tissue systems. In fact, the effects of gravity may explain why fish have a straight spine while humans have curved spines, a physiologic adaptation seemingly designed to offset and distribute the pull of gravity. Consequently, much energy is expended from birth to counteract the cumulative effects of gravity, which are more pronounced after injury and with aging. As such, a water-based environment might transiently liberate the body from the adverse effects of gravity. In the water, energy normally needed to resist gravity and maintain the human form in an upright, mobile, and functional position can instead be transferred to tissue repair and regeneration in the setting of injury or rehabilitation.
The use of water for therapeutic purposes has origins dating back to ancient Egyptian, Greek, and Roman civilizations. Today, water therapy encompasses a broad array of applications from supportive to therapeutic, and from recreational to rehabilitative. Hydrotherapy and water therapy both take advantage of the physical properties of water; however, the two approaches are very different. Hydrotherapy, a supportive, passive, adjunctive treatment used in nursing and therapy, refers to immersion of the body in a whirlpool or bath in an effort to use the properties of water, including temperature and pressure, to passively improve circulation and provide stress or pain relief (Mooventhan and Nivethitha, 2014). A commonly example is WATSU (Water Shiatsu), which involves the use of passive stretch and massage techniques, including palpation of acupressure points, performed in warm water (Schitter et al., 2015).
Water therapy, on the other hand, is an active form of physical and recreational therapy that engages the physical properties of water, including buoyancy, resistance, and hydrostatic pressure, to train and condition, actively rehabilitate injuries, and maintain health. This occurs by facilitating relaxation, decreasing restriction of movement, and unloading joints. In turn, these effects create a margin of therapeutic safety exceeding that of almost any other treatment setting (Becker, 2009). One water therapy method seen both in practice and literature is the Halliwick Method. First described in 1981, this method, also known as the Ten Point Program, incorporates some aspects of hydrotherapy but primarily involves active techniques to help clients increase stability and postural control and facilitate movement through sensory input and fluid mechanics imparted by water (Weber-Nowakowska et al., 2011).
RESEARCH ON WATER THERAPY: EXISTING LITERATURE AND FUTURE DIRECTIONS
Several recent systematic reviews have shown the value of water therapy. Although duration, frequency, components, and outcome assessments of individual therapy programs have been variable, consistent benefits have been shown in diverse patient populations, with few reported adverse events such as fatigue, anxiety, and chlorine sensitivity (Becker, 2009). In neurological injuries such as spinal cord injury, positive findings include improved physical function, physical fitness, and mobility (Li et al., 2017). Numerous studies have shown that therapeutic water exercise is a safe and efficacious modality for chronic musculoskeletal pathology such as low back pain (Waller et al., 2009). This is especially important for clients who are limited by weight-bearing components of land-based interventions. By naturally offloading pressure from joints, water provides an optimal environment for clients to exercise aerobically and at greater intensities than would be possible on land (Cuesta-Vargas et al., 2011). Water can also promote the body’s innate ability to heal itself. In clients with fibromyalgia, improvements were demonstrated in quality of life, stiffness, cardiovascular function, muscle strength, depression, anxiety, and sleep (Bidonde et al., 2014). Multiple studies have shown positive outcomes for cardiopulmonary clients related to exercise performance, body composition, skeletal muscle strength, and respiratory function (McNamara et al., 2013). In older adults, data suggest that water- based exercise is as effective as land-based exercise in improving physical functioning, with statistically significant improvements in muscular strength and endurance, balance, flexibility, and aerobic capacity (Waller et al., 2016).
The literature in exercise science has grown in support of water therapy; however, there remains significant heterogeneity in the types and protocols of treatments as well as in conditions treated. Therefore, reproducing these findings and generalizing these results to other populations is challenging. Additionally, although data has supported use of water therapy as an alternative to land-based therapy, there have been few studies illustrating the importance of using a combination of water and land therapy to improve outcomes. In one feasibility study of subjects rehabilitating surgical rotator cuff repair, the addition of water therapy to a land-based program significantly improved range of motion (ROM) measures at three and six weeks (Brady et al., 2008). In addition, a recent systematic review demonstrated that water therapy in combination with land-based therapy following hip or knee arthroplasty improves functional outcomes, ROM, and edema compared to land-based therapy alone (Gibson and Shields, 2015).
This combined water and land approach has the potential to help clients achieve greater therapeutic benefits and clinical outcomes. For example, while traditional rehabilitation on land may be more effective than water exercises at increasing strength postorthopedic surgery in isolation, the hydrostatic pressure and warmth of water can decrease pain, muscle spasms, and swelling and contribute to a faster recovery rate (Tovin et al., 1994; Zamarioli et al., 2008). One example of this combined approach to water and land therapy is TBM, which was studied in 2017 in clients with multiple sclerosis (MS). This study compared the effects of three 8-week programs including one land-based, one water-based, and one combined water and land-based program using TBM, on walking capacity in MS clients. Although limited by a small cohort size of 31 clients, the study found that while all three groups significantly increased their walking capacity, this improvement was significantly higher in the combined water and land program using TBM, compared to water-based exercise alone (Ghaffari, 2017). In addition, TBM has been used with success in pediatric populations, particularly in those who may have limitations walking or moving on land such as clients with cerebral palsy, spinal bifida, or paraplegia (Ray and Galloway, 2006).
As the general population ages and lives longer with chronic disease and related disability, more individuals may be precluded from participating and excelling in land-based therapy or exercise alone, despite its known benefits (Schutzer and Graves, 2004). In this article, and as a general approach to rehabilitation, conditioning, and training, the use of a combined water and land program is encouraged. In the next section, clinical experiences and perspectives are provided to demonstrate that using water as a modality can have a synergistic affect when combined with a land-based program, both theoretically and practically.
AN EXAMPLE OF COMBINED WATER AND LAND THERAPY: THE BURDENKO METHOD
The use of water therapy is not a new concept, but identifying and applying a water-based program can be difficult due to heterogeneous approaches and variable availability of educational materials. Table 1 provides a summary of several common hydrotherapy and water therapy methods. To provide one example of a potential framework, described below are the basic principles and components of TBM, a system developed over four decades ago which has been studied in research literature and has combined exercise in both water and land to effectively treat clients in a variety of clinical settings, as well as athletes from all levels of training, including professional sports players, Olympians, and dancers (Burdenko et al., 2017). The program focuses on the principle of fitness intelligence, which is founded on the following tenets: exercise is performed in both shallow and deep water in the vertical position; exercise changes starting positions in regards to postural control and multidirectional stability; exercise is practiced at different speeds (slow, medium, fast); exercise is performed in multiple directions (forward, backwards, laterally) and includes navigating turns, jumping, and landing; exercise pays close attention to body alignment; finally, exercise keeps the client directly involved in the rehabilitation, conditioning, and/or training process, which can be choreographed to become a personalized routine that can be continued outside of the therapy setting.
Any effective water-based exercise derives its benefits from the unique properties conferred by water. One of these is buoyancy, the upward, anti-gravity force of the density of a fluid acting on an immersed object while holding it up. When we enter water, this pressure counteracts the downward force of gravity, helping relieve the body of compression and pain. The deeper we progress into water, the less pressure is exerted by gravity. Gravitational force is reduced by 30% at knee-level and 50% at waist-level, and at our neck we experience reduced weight bearing of approximately 90% (Harrison et al., 1992). By reducing pressure on the spine and other weight-bearing joints, buoyancy, combined with hydrostatic pressure, provides natural vertical traction that can decompress and provide mobility to previously stiff and painful joints.
It is also important to stress that vertical position is functional position, both in water and on land. Our bipedal anatomy is designed to hold us upright and move with maximum efficiency and stability while on land. However, in the presence of pain or injury, our bodies develop poor posture, gait deviations, and decreased mobility. Beginning an exercise program in deep water in the vertical position is recommended, with the goal of promoting and restoring the body’s natural alignment. In order to achieve this, the optimal degree of buoyancy would allow the client to maintain a head-out-of-water position in the deep end while encouraging relaxation of the body. Using an appropriate buoyancy device is key – buoyancy vests and cervical collars properly distribute buoyancy forces and increase mobility in the water and traction on the joints, leading to better alignment and less pain. Clients should be able to perform exercises without having to fight the device, and devices may need to be adjusted for each exercise or individual, such as a lean body mass requiring more buoyancy support. Conversely, using the wrong buoyancy device, such as a foam noodle, can promote an asymmetrical support structure and increase the body’s displacement, taking it out of alignment and disrupting the center of buoyancy.
Keeping in mind the principles above, the main goal of TBM is to engage in exercises that promote six essential qualities in the water and land (Fig. 1): balance, coordination, flexibility, endurance, speed, and strength. In contrast to solely land-based programs, TBM focuses on the whole body, with special attention on activating or relearning proper movement of injured areas through exercises that also normalize the entire system. Each principle that is taught in the water can be translated to the land. Maintaining one’s body in the vertical position in the water can lead to improved alignment and postural stability while walking on the ground. The extra resistance of water allows clients to grade their own levels of resistance and progress more pain-free, while also enabling us to recruit muscle fibers and motor units more actively than could be achieved on land.
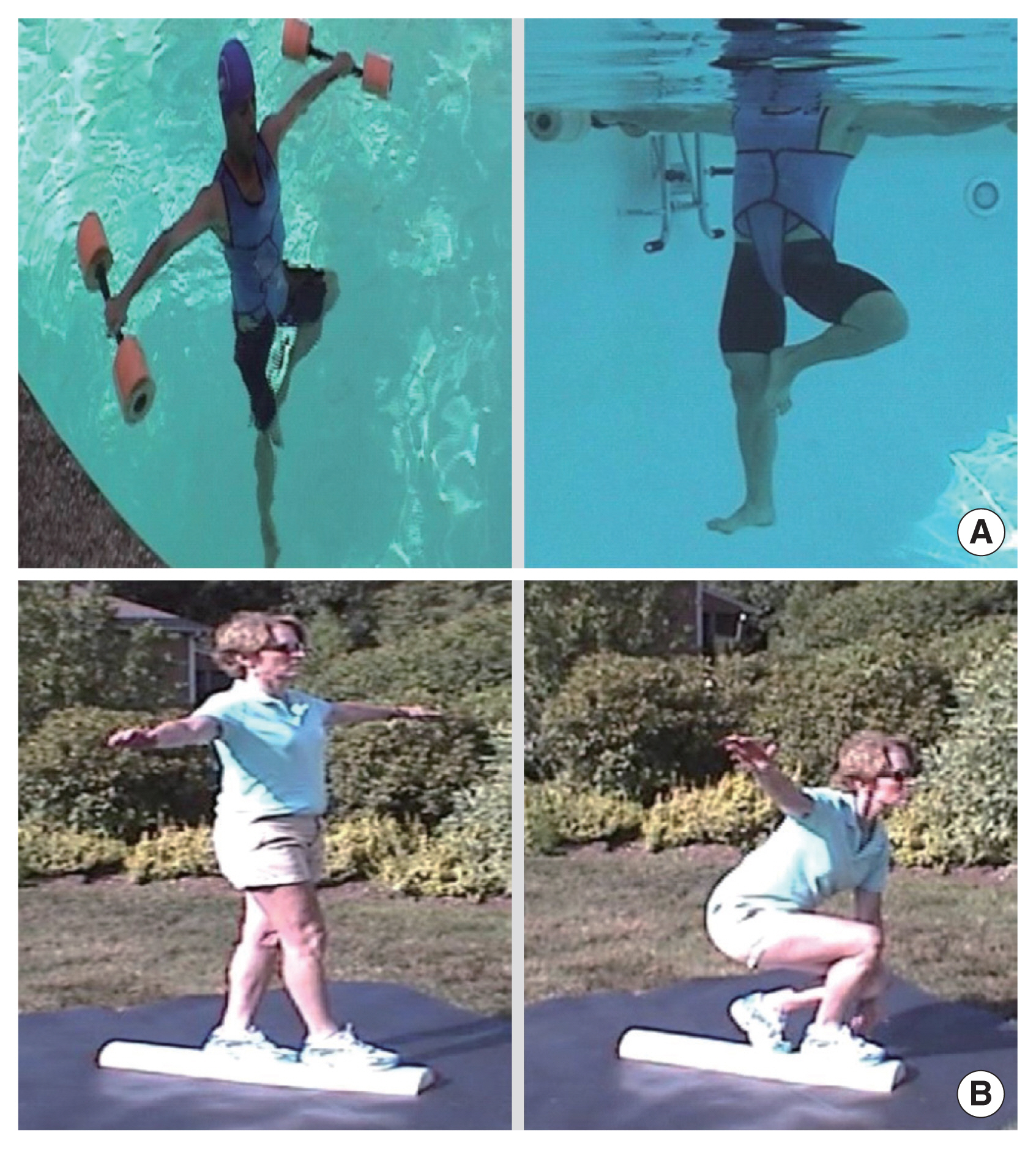
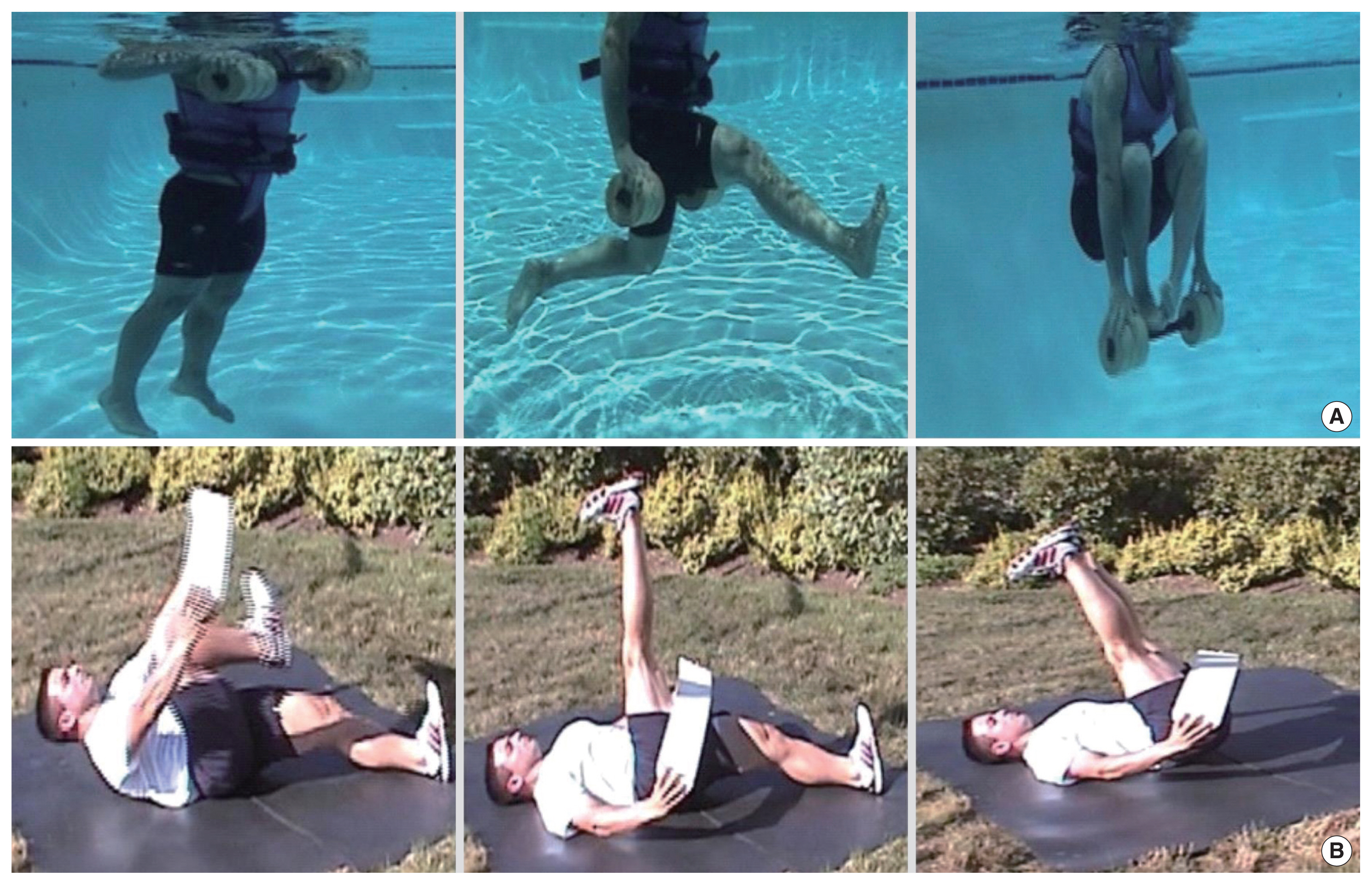
The first foundational quality is balance. This refers not just to balance required to stay upright while in the standing position, but also balance of the entire body and its systems. The right amount of balance allows us to maintain homeostasis, tolerate everyday changes and stressors, and remain resilient to disease and injury. Teaching balance in the water (Fig. 2) seeks to provide greater freedom with pain-free ROM and lays the foundation for subsequent learning of exercises. The second quality is coordination. Proper movement involves coordinated, controlled contraction and relaxation of the musculoskeletal system, while discoordination can predispose to stiffness and injury. Through coordination exercises (Fig. 3), clients can regain control over their injured areas and understand how each body part functions individually and as part of a group. The third quality is flexibility (Fig. 4). In traditional rehabilitation, flexibility is often the first component addressed. However, clients can best achieve proper, sustained flexibility if they engage in active movements after a good foundation of balance and coordination has been established.
To provide readers with additional information regarding the example exercises listed above, a supplementary file has been made available (Supplementary material). This document details the starting position, directions, key elements, and tips for each exercise. General information regarding water depth, temperature, number of repetitions, and limitations and precautions for implementing exercises in the water is also discussed. Finally, a link to publicly accessible videos is provided for readers’ benefit.
Fourth is the quality of endurance, giving clients the ability to safely perform exercises for increasingly longer periods of time. Without the prior qualities, clients may experience biomechanical breakdowns or injuries when fatigue settles in as the result of excess energy expended on maintaining balance, poorly coordinated movements, or muscles being forced to work through unsafe ROM. Speed comprises the fifth quality and focuses on clients’ ability to effectively use the entire body and its individual parts while changing direction and velocity. These exercises challenge clients’ baseline physiology and stress the cardiovascular system to improve exercise capacity. Finally, the sixth quality is strength. This can be defined more as the ability to resist pressure in all directions in space, rather than power production alone. In this approach, strength training exercises involve controlling clients’ center of gravity on land, and center of buoyancy in water, thus allowing them to safely progress to resisting increasing loads on the human body and returning it to prior level of function.
As the body learns and practices the exercises, while employing the six essential qualities, the central nervous system also adapts and evolves, reflecting the strong positive relationship between physical exercise and central nervous system health (Dustman et al., 1994). Exercise-induced improvements in learning and memory have been associated with increased neural synaptic plasticity and hippocampal volume, suggesting that exercise may improve brain function and slow decline of cognition with aging (Erickson et al., 2011). In the short-term, challenging the body and mind to learn multidirectional stability, dynamic postural control, and varying degrees of gravity in the water prevents adaptation of the body to repetitive exercises and allows clients to remain engaged in their own rehabilitation and training process.
CASE SUMMARY
Clients from all walks of life can benefit from a combined water and land program. In one case, when Olympic figure skater Nancy Kerrigan lost her ability to skate after acute trauma, she used exercises from TBM to relearn her routine in the water before returning to the ice and ultimately claiming the silver medal in 1994. Conversely, an 80-year-old with debilitating right hip osteoarthritis achieved his personal goals with a combined approach in the following brief case summary. He was referred after reporting no improvement with traditional land therapy; he was limited to ultrasound and passive ROM exercises due to pain exacerbation, and stopped after six sessions. He was not a candidate for hip arthroplasty due to cardiac and renal comorbidities. At baseline, he ambulated with a rolling walker with partial weight bearing on the right, had severely limited ROM due to pain, and had poor mobility even in the home. He was deconditioned to the point where he required a chairlift in and out of water, as well as a therapist just to stay vertical and maintain his center of buoyancy. However, he reported pain relief in the pool from the onset and improved ROM in water and land exercises, and over the course of six sessions, was able to touch down at neck, then chest-depth in the deep end. After ten sessions, he was walking in deep water primarily without therapist assistance, and was using pool stairs rather than the chairlift. After therapy sessions, he reported (a) average carryover of 50% pain reduction the next day; (b) improved mobility during transfers; and (c) ability to navigate a flight of stairs at home daily.
CONCLUSIONS
In conclusion, the combination of water and land enhances exercise synergistically. Water is therapeutic, safe, and provides a unique environment to address physical impairment and pain, impart more freedom of movement, and restore healthy biomechanics, all of which can be translated to further progress on land and vice versa. We hope this perspective will be part of a continued effort towards developing exercise programs using both water and land to optimize results in rehabilitation, conditioning, and training, both in practice and in research.