Effects of multimodal cognitive exercise program on cognitive function, bone density, blood lipid, fitness, and depression in old women with mild cognitive impairment
Article information
Abstract
The purpose of this study is to verify the effects of participation in 12-week multimodal cognitive exercise program on cognitive function, bone mineral density, blood lipids, senior functional fitness, and depression of the old women with mild cognitive impairment and osteopenia. As a result, the exercise group showed significant effects in cognitive function, depression, bone mineral density, blood lipid, lower extremity flexibility, upper extremity flexibility, dynamic balance, and body endurance. Such results prove that multimodal cognitive exercise program is an effective interventional exercise program for improving cognitive function in the old women with mild cognitive impairment.
INTRODUCTION
Mild cognitive impairment (MCI) is the transitional stage between normal cognitive function and dementia. Because 5%–20% of them are changed to dementia every year, they need to get the intensive-preventive care (Langa and Levine, 2014). Exercise is one of the strongest protective life elements that could reduce the risk of dementia (Livingston et al., 2017). Especially, exercise can delay the time for the elderly with MCI to have dementia by average 3–5 years, so it is important to select the elderly with the initial symptoms of dementia and then to present the accurate exercise guidelines for them.
The fitness in old age is highly related to cognitive function (Alfaro-Acha et al., 2007; Kang et al., 2022; Sattler et al., 2011). And some recent researches present that the low bone mineral density is related to the transition from MCI to Alzheimer’s (Peng et al., 2016; Zhou et al., 2014). Thus, the decline of health-related fitness and bone mineral density of the elderly with MCI has huge effects on dementia as an initial sign of dementia, so the exercise intervention through early detection is important. Also, when the level of blood total cholesterol (TC) is higher, the risk of MCI is high. And the elderly with MCI show high TC or low-density lipoprotein cholesterol (LDL-C) (Lesser et al., 2001; Yaffe et al., 2002). When the degree of depression is higher, it is highly possible for the elderly to be transferred to dementia, so the application of proper exercise to the elderly with MCI is necessary in the preventive aspect.
The recent researches related to the effects of exercise on the improvement of cognitive function present the results in which the multimodal intervention exercise program is more effective than a single exercise (Karssemeijer et al., 2017). Concretely, it is reported that the exercise program combined with aerobic exercise and resistance exercise brings about greater improvement of cognitive function than a single exercise program (Scherder et al., 2014; Young et al., 2015), and that the program applying exercise and cognitive training together is effective for the prevention of Alzheimer’s (Yu et al., 2018).
This shows that the multimodal exercise is more effective for the prevention of dementia in old age than the application of a single exercise, and especially, the multimodal intervention of exercise and cognitive training together are very important preventive measures that cannot be ignored. Despite many researches reporting that the exercise strengthens cognitive function, there should be continuous researches on the basic mechanism of the relation between exercise and cognitive function. In particular, recently, results have been suggested that bone health and cognitive impairment in the elderly are related, and the low bone density in elderly women is an initial indicator of cognitive impairment. Therefore, it is necessary to develop a complex exercise program that prevents a loss of bone density in the elderly and improves cognitive function, and study to prove its effectiveness is also continuously needed.
Therefore, based on recent studies showing that bone health is related to cognitive impairment, this study aims to apply a complex exercise program to elderly women with osteopenia and osteoporosis lesions as well as MCI, and to verify its effectiveness. The final purpose is to examine whether a complex exercise program is cognitively, psychologically, and physically effective for the elderly, and to provide a complex exercise program necessary for the old women with MCI.
MATERIALS AND METHODS
Participants
In the process of recruiting the subjects, this study selected total 24 old women diagnosed as MCI in the results of conducting the cognitive function test targeting the old women of Senior Welfare Center in Goesan-gun, Korea and also diagnosed as osteopenia (T score: −1.0 to −2.5) or osteoporosis (T score: −2.5 or lower) in the results of bone mineral density test. Through the medical history survey and interview, they were classified into exercise group (N=10) and control group (N=10), and their physical characteristics are as Table 1. This study was approved by the Institutional Review Board of Jungwon University (approval number: 1044297-HR-202006-005-03).
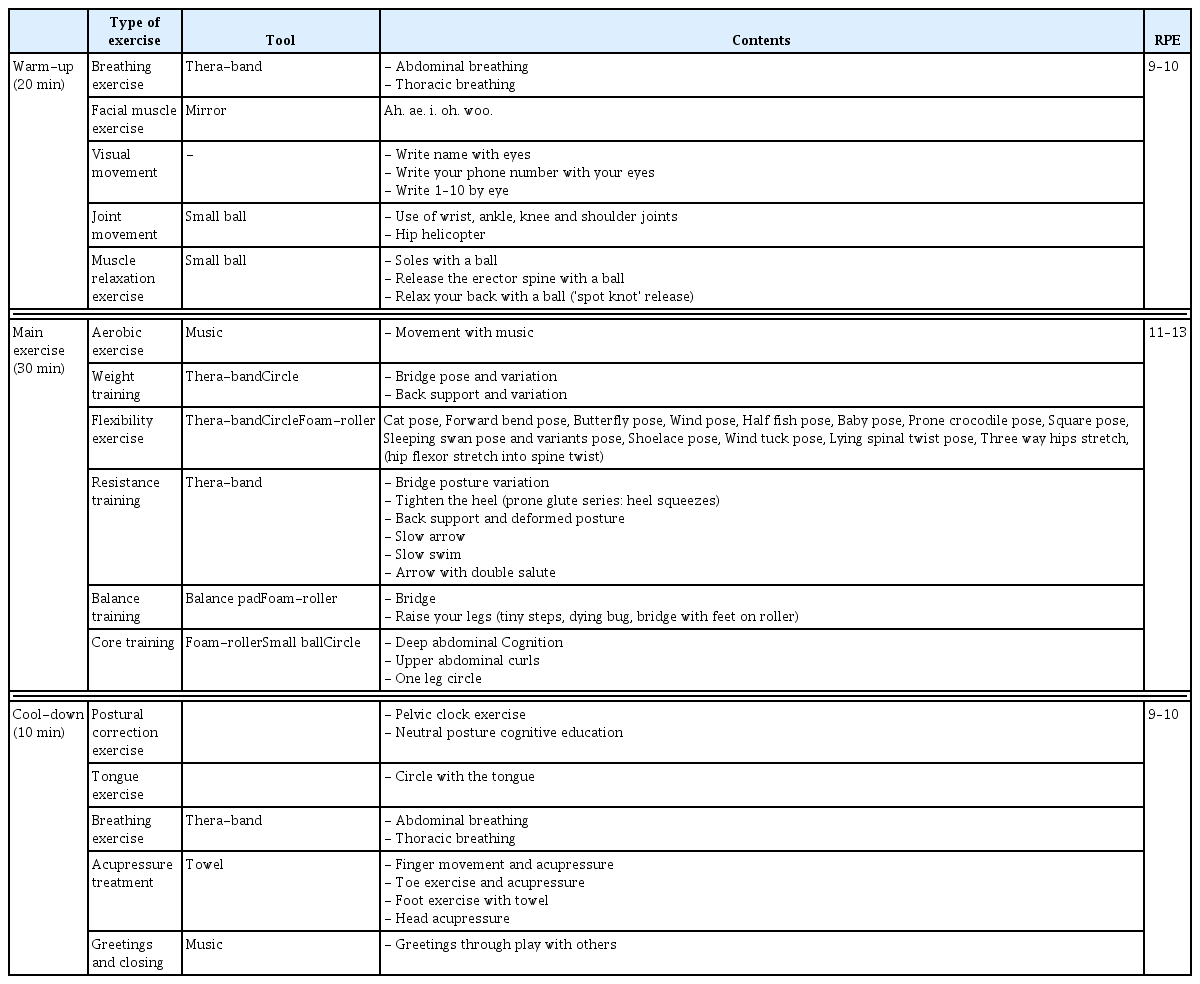
Exercise program
This exercise program was developed on the basis of ‘ADDIE Model.’ As a general model of instructional systems development, ADDIE Model is composed of analysis, design, development, implementation, and evaluation. The developed program is shown in Table 2.
Body composition and blood pressure
As the variables of body composition, the height, weight, and body mass index were measured through Inbody 720 (Biospace, Seoul, Korea). The measurement was conducted after urinating 30 min before the measurement and resting for 5 min in a comfortable state. The measurement was performed according to the explanation of the measurer while looking at the front without wearing shoes and removing belongings. Blood pressure was measured by using the automatic blood pressure monitor FT-500 (Jawon Medical, Gyeongsan, Korea) after taking a rest for 10 min in a sitting posture. By repetitively measuring it twice at 2-min interval, the mean value was recorded.
Senior fitness test
Regarding the senior functional fitness, the functional fitness test was conducted by following the manual suggested in the senior fitness test developed by Rikli and Jones (1999). The test is composed of total 6 items such as lower extremity muscle strength, upper extremity muscle strength, lower extremity flexibility, upper extremity flexibility, agility with dynamic flexibility, and general endurance. Lower extremity muscle strength was measured once when the subjects made both arms in the shape of an X and stood up from a chair in the correct posture. Upper limb muscle strength was measured once when a 2.2-kg dumbbell was lifted and lowered. Lower extremity flexibility was measured by touching the toes with both hands while sitting on a chair, and measuring the cm between the outstretched finger and the tip of the toe. For upper extremity flexibility, one hand was placed behind the shoulder and the other arm was bent downward so that both hands were clasped behind the back. Measured in cm between the middle fingers. Dynamic balance was measured by walking from the starting point of 2.44 m and the time from returning to sitting on a chair. body endurance records the number of steps taken in place for 2 min.
Bone mineral density test
Bone mineral density was measured by ultrasonic bone mineral density meter SONOST-2000 (Osteosis, Seoul, Korea). In this study, the density was calculated by using the bone quality index. As for the measurement method, the bone density index was measured by attaching the Achilles’ tendon area to the sensor. Following the criteria specified in the World Health Organization as the diagnosis criteria of bone mineral density, the subjects were classified into normal when T score was higher than −10, into osteopenia when T score was in −10 to −25, and into osteoporosis when T score was lower than −25. As for the measurement method, the bone density index was measured by attaching the Achilles’ tendon area to the sensor.
Lipids test
The research participants were told to keep the empty stomach for more than total 12 hr by fasting from 7 p.m. on the night before the test, and the test was performed in the next morning. In the blood lipids test, the blood sample that was taken in the finger tip method was measured through the equipment called Cholestech LDX (Alere, Oslo, Norway). After taking the blood sample (about 35 μL) from the index fingertips of research participants, the kit containing the blood sample was inserted in the measurement equipment for analysis. Following the manufacturer’s protocol, the figures of triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), LDL-C, and TC were automatically calculated 5 min later (Marcus et al., 1992).
Korean version of Mini-Mental State Examination for dementia screening
The subitems of Mini-Mental State Examination for dementia screening (MMSE-DS) are composed of total 19 items within five test areas such as orientation of time with place, affixation of name, recollection, attention with calculation, language function, and orientation which is divided into time and place is comparatively analyzed by classifying it into six areas. Based on total score (30), the subjects with 24 points or higher are regarded as normal; the subjects with 20–23 points as suspected dementia; and subjects with 19 points or lower as determinate dementia. In the additionally-prepared space accompanied by a social worker and nursing student within the professionally-trained institution, the test was conducted in the individual-interview form. The reliability of the scale is 0.935 (Kim et al., 2010).
Geriatric depression scale
For the measurement of depression, this study used the Korean version of short form geriatric depression scale in Korea which was adapted into Korean version by Bae and Cho (2004) developed by Yesavage et al. (1983), composed of total 15 items. Each item is composed of 0–1 point, and the lower score means the lower degree of depression.
Statistical analysis
The number of subjects in this study was calculated using the G-Power ver. 3.1 (University of Dusseldorf, Dusseldorf, Germany) program. We performed a two-sample t-test with a significance value (α) 0.05, power 85%, and effect size 1.2. According to the probabilistic calculations, 24 old women with MCI used as the minimum sample size. Regarding the general characteristics of the research participants, descriptive statistics were calculated, and as to the normality of the measurement variable, a nonparametric test was conducted after checking variability through a Kolmogorov–Smirnov test. The Mann–Whitney U-test was conducted to compare the difference in the variance between the two groups. Statistical significance was set at P<0.05. Statistical analyses were conducted using IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA).
RESULTS
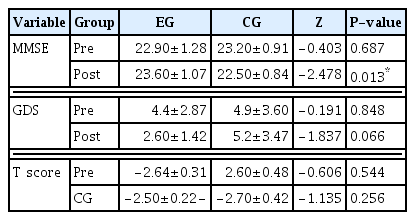
Table 3 shows the results of analyzing the difference in the average change before and after of the two groups by Mann–Whitney U-test. It can be seen that there is a statistically significant difference between the two groups only in cognitive function (P<0.05).
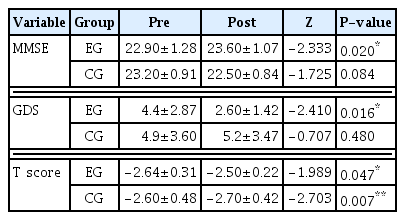
Table 4 shows the results of analyzing the average difference before and after each group’s experiment by Wilcoxon test. In the cognitive function test, there was a significant increase from 22.90± 1.28 to 23.60±1.07 in the exercise group (P<0.05), but there was no significant change in the control group. Geriatric depression scale showed a significant decrease from 4.4±2.87 to 2.60± 1.42 in the exercise group (P<0.05), but there was no significant change in the control group. In the case of T score, it decreased significantly from −2.64±0.31 to −2.50±0.22 in the exercise group (P<0.05), and significantly increased from −2.60±0.48 to −2.70± 0.42 in the control group (P<0.01).
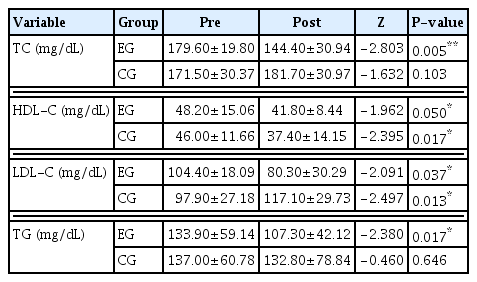
Table 5 shows the results of analyzing the difference in the average change before and after of the two groups by Mann–Whitney U-test. It can be seen that there is a statistically significant difference between the two groups in TC and LDL-C (P<0.05).
Table 6 shows the results of analyzing the average difference before and after each group’s experiment by Wilcoxon signed ranks test. In the case of TC in the blood lipid test, there was a significant decrease from 179.60±19.80 to 144.40±30.94 in the exercise group (P<0.01), but there was no significant change in the control group. HDL-C showed a significant decrease from 48.20± 15.06 to 41.80±8.44 in the exercise group (P<0.05), as well as a significant decrease from 46.00±11.66 to 37.40±14.15 in the control group (P<0.05). In the case of LDL-C, it decreased significantly from 104.40±18.09 to 80.30±30.29 in the exercise group (P<0.05), and significantly increased from 97.90±27.18 to 117.10±29.73 in the control group (P<0.05). In the case of TG, it decreased significantly from 133.90±59.14 to 107.30± 42.12 in the exercise group (P<0.05), and there was no significant change in the control group.
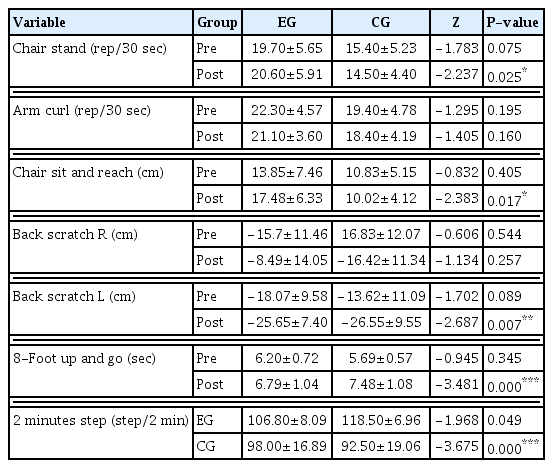
Table 7 shows the results of analyzing the difference in the average change before and after of the two groups by Mann–Whitney U-test. It can be seen that there is a statistically significant difference between the two groups in lower extremity flexibility (P<0.05), lower extremity flexibility (P<0.05), upper extremity flexibility-L (P< 0.01), dynamic balance (P<0.001), body endurance (P<0.001).
Table 8 shows the results of analyzing the average difference before and after each group’s experiment by Wilcoxon test. In the case of lower extremity muscle strength, increased from 19.70± 5.65 to 20.60±5.91 in the exercise group, but there was no statistically significant difference. On the other hand, the control group significantly decreased from 15.40±5.23 to 14.50±4.40 (P<0.05). There was no statistically significant change in upper limb muscle strength in both the exercise group and the control group. In the case of lower extremity flexibility, it increased significantly from 13.85±7.46 to 17.48±6.33 in the exercise group (P<0.01), and there was no significant change in the control group. Upper extremity flexibility R showed a significant increase from −15.7±11.46 to −8.49±14.05 in the exercise group (P<0.05), and there was no significant change in the control group. Upper extremity flexibility L showed a significant increase from −18.07± 9.58 to 13.62±11.09 in the exercise group (P<0.05), and there was no significant change in the control group. Dynamic balance a significant decrease from 6.20±0.72 to 5.69±0.57 in the exercise group (P<0.01), and significantly increased from 6.79±1.04 to 7.48±1.08 in the control group (P<0.01). body endurance a significant increase from 106.80±8.09 to 118.50±6.96 in the exercise group (P<0.01), and there was no significant change in the control group.
DISCUSSION
There have been continuous researches applying double tasks or multimodal exercise program focusing on the improvement of cognitive function of the old women with MCI. After it was recently revealed that the low bone mineral density would be related to the transition from MCI to Alzheimer disease, there have been many researches related to it (Peng et al., 2016; Zhou et al., 2014). Thus, this study aims to apply the multimodal exercise program to the elderly women with low bone mineral density and MCI, and then to verify its effects.
The 12-week multimodal cognitive exercise program showed significant effects on cognitive function, bone mineral density, fitness, blood lipids, and depression of the elderly with MCI. Some existing researches also report that the regular exercise improves the bone mineral density of ordinary elderly women (Englund et al., 2005). In a study by Benedetti et al. (2018), aerobic exercise does not improve bone mass, and for osteoporosis patients, it is effective for bone mass to do multicomponent exercise, including aerobics, strengthening, progressive resistance, balancing and dancing. The complex exercise program of this study also showed a positive effect on improving bone density in the old women with MCI.
In addition, it has been known that aerobic exercise lowers depression in the elderly and has a positive effect on cognitive symptoms (Fleg, 2012; Imboden et al., 2020). However, recent studies have proven its effectiveness through multicomponent exercise intervention (Jeong et al., 2021). Through this study, it was also confirmed that the multimodal cognitive exercise program is an effective exercise in lowering depression and enhancing cognitive function of elderly women with MCI. This suggests that exercise program that should be provided to the elderly reduce their depression, improve bone density and cognitive function is exercise that include multicomponent elements. Therefore, based on the results of this study, it is necessary to come up with a plan to more actively spread the multimodal cognitive experience program to the elderly.
Researches by Dannhauser et al. (2014) also report that the multimodal cognitive improvement program is effective for improving the cognitive function of elderly women, and the complex multimodal activity program is effective for physical health, fitness, and cognitive function, which is supporting the results of this study. However, in a recent study of Ahn and Kim (2023), through systematic literature review and meta-analysis, the opposite results can be seen that aerobic exercise and resistance exercise are effective in improving overall cognitive function, but complex exercise and nerve exercise are not. Therefore, it is necessary to continuously present study results based on strict study design in the future.
Lastly, many researches are mentioning the relationship with blood lipids as the risk factor of MCI (He et al., 2016; Kivipelto et al., 2001). In case of MCI, the level of TC is highly shown (He et al., 2016). The increase of blood TC increases the secretion of beta amyloid that causes dementia. When the level of blood HDL-C is higher, the risk elements of dementia such as neocortex nerve fiber and hippocampus are decreasing (Coelho et al., 2013). In this study, the 12-week multimodal cognitive exercise program had a significant effect on blood lipids. However, as there are no consistent reports on the role of lipid level in cognitive function, there is a room for controversy, so it would be necessary to continuously conduct additional researches (He et al., 2016; Li et al., 2004; Mielke et al., 2005).
In conclusion, this study verified that the multimodal cognitive exercise program would be significant exercise for improving the cognitive function and bone mineral density of old women with low bone mineral density and MCI. Furthermore, this study verified its significant effects on blood lipids, lower extremity flexibility, upper extremity flexibility, dynamic balance, and general endurance, and significant effects on the improvement of depression. In future studies, it will be necessary to compare and analyze the effectiveness of aerobic exercise, resistive exercise, and a complex exercise program by increasing the sample size.
ACKNOWLEDGMENTS
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2017S1A5B5A02025639).
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.