The optimal cutoff score of the 2-min step test and its association with physical fitness in type 2 diabetes mellitus
Article information
Abstract
This study was carried out to evaluate sensitivity, specificity, and test cutoff score to predict cardiorespiratory fitness by using the 2-min step test (2MST) in patients with type 2 diabetes mellites (DM). The association of the 2MST and physical fitness tests including a 6-min walk test (6MWT), a 5 time sit-to-stand test (FTSST), and leg strength in the form of a leg performance test were also investigated. This study was cross-sectional and conducted in 100 type 2 DM patients. Patients were screened through health questionnaires, medical illness, general characteristics, and physical fitness tests; 2MST, 6MWT, FTSST, and leg strength. Blood was collected for assessment of fasting blood sugar and lipid profiles. The number of steps in the 2MST was positively correlated with the distance of the 6MWT (r=0.6995, P<0.0001) and leg strength (r=0.4292, P<0.0001). 2MST was negatively correlated with time to perform the FTSST (r=−0.405, P<0.0001). Moreover, this study established the optimal cutoff score of the 2MST at ≤61 steps with 92.24% sensitivity, and 81.36% specificity to predict cardiorespiratory fitness in type 2 DM patients. Our findings indicate that the 2MST may be used as a predictor for walking capacity, leg strength, and ability to change position from sitting to standing in type 2 DM. In addition, this result may imply that patients with type 2 DM performing the 2MST at less than 61 steps was significantly associated with decreased cardiorespiratory fitness.
INTRODUCTION
Diabetes mellitus (DM) is a chronic disease which is an important cause of neuropathy, retinopathy, nephropathy, diabetic foot ulcers, hypertension, coronary arterial disease, and stroke (Hou et al., 2020). The quality of life of patients with DM deteriorates when commodities coexist or complications start to develop (Trikkalinou et al., 2017). Physical activity is one of the key components concerning quality of life. It is clear that physical activity plays an important role in improving quality of life and maintaining cardiorespiratory health and reducing cardiovascular mortality among all ages (Jakovljevic, 2018; Koo et al., 2016). The previous cohort of patients with type 2 DM who reported being inactive reported cardiorespiratory fitness decline (Palakodeti et al., 2015).
A physical fitness test is a test designed to evaluate physical performance such as, agility, flexibility, strength, and endurance. A field test is used to measure cardiopulmonary, musculoskeletal performance, balance, and coordination in clinical practice. It is commonly applied to design rehabilitation protocols in varying pathological conditions. The 2-min step test (2MST) is a screening implement to assess cardiorespiratory fitness or aerobic capacity (Rikli and Jones, 1999b). It has been widely used in older adults with or without pathologies (Bohannon and Crouch, 2019). Currently, there are many reasons supporting the performing of the 2MST, such as there is no expensive equipment, the test only takes a few minutes, it is tolerable for patients, and it can be utilized as an alternative measuring test in conditions with limited space to perform the 6-min walk test (6MWT). This is especially appropriate in a community or in elderly persons living at an old people’s home (Chaturvedhi, 2021; Haas et al., 2017). Consequently, the 2MST may be an alternative to a field test for measurement of aerobic performance, planning of exercise prescription, and determining the category of normal and poor cardiorespiratory fitness in type 2 DM. Although maximal oxygen consumption is commonly applied as a key point of reference of cardiorespiratory endurance capacity measurement, the participant requires strong motivation to reach the exhaustion state under a high intensity load. Accordingly, it is inappropriate for individuals with medical conditions as well as elderly individuals not in the habit of exercise.
Cardiorespiratory endurance capacity and muscle strength are a fundamental component of physical fitness and functional activities. Numerous research articles have reported that physical fitness worsens in DM patients, for instance, a decline in muscular strength and endurance (Gordon et al., 2009; Lee et al., 2018; Palakodeti et al., 2015). Interestingly, the distance of the 6MWT which is an indirect method as a necessary estimation of oxygen consumption, showed a moderate association with maximal oxygen uptake in type 2 DM (Lee, 2018). In addition, the distance of the 6MWT was positively correlated with the number of steps performed during the 2MST, quadriceps strength, and peak oxygen consumption in patients with heart failure (Wegrzynowska-Teodorczyk et al., 2016). Moreover, during the last 5 years the researcher reported that the 2MST was valid, reproducible, and a sufficiently sensitive test to predict cardiorespiratory endurance capacity in healthy, active, sedentary, chronic obstructive pulmonary disease patients, and type 2 DM participants (Haas et al., 2017; Lee, 2018; Nogueira et al., 2021). Thus, the 2MST may be considered as an alternative to the 6MWT to evaluate cardiorespiratory endurance in participants with a limited capacity to perform the 6MWT.
The 6MWT test cutoff point was identified to differentiate between normal and low cardiorespiratory fitness patients (Chetta et al., 2006; Jones and Rikli, 2002; Lord and Menz, 2002; Pires et al., 2022; Wetzel et al., 2011) in addition to the 2MST test cutoff point which was identified to differentiate between active and sedentary individuals (Nogueira et al., 2021). However, cardiorespiratory endurance fitness cutoff score of the 2MST in patients with type 2 DM was not reported. Therefore, the purpose of this study was to evaluate sensitivity, specificity, and test cutoff score to predict cardiorespiratory endurance fitness levels in patients with type 2 DM. The association of 2MST and physical fitness tests includes the 6MWT, leg strength, and the 5 time sit-to-stand test (FTSST) which is a leg performance test.
MATERIALS AND METHODS
Study designs and participants
This cross-sectional study was conducted in 100 patients with type 2 DM, living in six rural communities, Phayao province, Thailand. Placards containing the study details were posted through staffs at the primary health care centers. Patients who had attended the primary health care services and interested in participating in the study contacted a staff or a research assistant by phone and Line application. The eligibility criteria included the following: patient was diagnosed with type 2 DM by a physician at least one year prior, and a body mass index (BMI) <30 kg/m2. Patients who had a history of orthopedic or surgical disease interfering with walking, a recent infection, unstable angina, a myocardial infarction during the month prior, resting heart rate (HR) >120 bpm, resting systolic blood pressure (SBP) >180 mmHg or diastolic blood pressure (DBP) >100 mmHg, were excluded. This research was performed following the Declaration of Helsinki principles. The Human Research Ethics Committee of the University of Phayao (No.2/165/2017) approved the study. Informed consent was obtained from all participants prior to participation. The minimum sample size (80 participants) was calculated for a diagnostic study with variables set as a power of test at 90%, a P-value at 0.05, and sensitivity from a pilot study (n=40) at 71%.
Study protocols
The experimental protocols were divided into two visits. On the first visit, participants were determined using health questionnaires consisting of the following items: general information, medical illness, history of exercise participation and supplementation intake, and mental health, in addition to a physical examination, which measured body mass, height, BMI, blood pressure (BP), and HR. Blood was also collected to assess fasting blood sugar (FBS), and hemoglobin A1c (HbA1c). Subsequently, a physical fitness test, a FTSST, and a 2MST were measured in each participant with a 30-min rest between tests. Later the following week, participants were evaluated leg strength and performed a 6MWT.
5 Time sit-to-stand test
The FTSST was commonly employed to evaluate functional lower extremity strength, transitional movements, balance, and fall-risk in the elderly (Schaubert and Bohannon, 2005). Briefly, the researcher first demonstrated the correct maneuver, then the participant was asked to rise from a chair 5 times as quickly as possible with their arms folded across their chest. The chair was of a standard height (0.43 m) without armrests. Two trials were performed with approximately a 1-min rest between each trial. The values of time in the two maneuvers were averaged and recorded. Test-retest reliability was determined from a subset of 30 subjects who took part in the trial.
2-Min step test
The 2MST is a cardiopulmonary endurance test commonly used in older adults. The maximum number of steps in 2 min is obtained to determine endurance capacity. Briefly, prior to beginning the test, the researcher first demonstrated the correct maneuver. Then, vital signs, leg fatigue, and dyspnea score were recorded in the sitting position for each participant. Besides that, the height of the iliac crest and patella were measured and marked on a wall. Then, a piece of tape was stuck on the wall at half the distance between the two. Each participant was instructed to step up and down and raise each knee to the mark on the wall as many times as possible during the 2-min period. The researcher counts only the steps of the right knee which reach the minimum marker (Rikli and Jones, 1999b), while assisting in case of a loss of balance. At the end of the test, vital signs, leg fatigue, and dyspnea score were immediately recorded.
Leg strength test
Maximal isometric output of lower limb muscle strength was measured by a strength dynamometer according to a standard assessment protocol (Bandinelli et al., 1999). In brief, the participant was asked to stand on the base of the dynamometer with feet shoulder width apart. Participants were required to keep their arms hanging straight down in order to hold the center of the bar with both hands - with the palms facing toward the body. The researcher adjusted the chain so that the knees were bent at approximately 110 degrees. Then, the participant pulled as hard as possible on the chain while attempting to straighten their legs and keeping the arms straight without bending the back. The test was performed twice with the maximum performance recorded.
6-Min walk test
The 6MWT is widely applied for assessing functional capacity (Crapo et al., 2002; Du et al., 2017). In brief, the participant was required to rest in the sitting position for 5 min with vital signs, leg fatigue, and dyspnea score subsequently recorded. Participants were instructed to walk along a flat corridor marked with a 30-m track pathway as fast as possible, without running, for 6 min. The same variables were assessed again immediately following test termination.
Statistical analysis
Data were expressed as mean±standard deviation. Statistical analysis was performed using the Stata 11.5.1 (StataCorp LLC, College Station, TX, USA). Descriptive statistics including means, standard deviations, and percentages were computed for participant characteristics. Physiological response (BP, HR, and oxygen saturation) differences between male and female were measured using Student t-test, and the differences between the 2MST and 6MWT were evaluated using paired t-test. Leg fatigue and dyspnea score were measured using the signed-rank test. Moreover, the Pearson correlation coefficient was employed to investigate the correlation between the number of steps from the 2MST, distance of the 6MWT, and time from the FTSST. The correlation was considered as weak if r was <0.50, moderate if r was 0.50–0.70, and good if r was >0.70. Finally, the receiver operating curve (ROC) was utilized to record cutoff score, sensitivity, specificity, and area under the curve (AUC) of the 2 MST. The level of statistical significance was set at P<0.05.
RESULTS
General characters of all participants
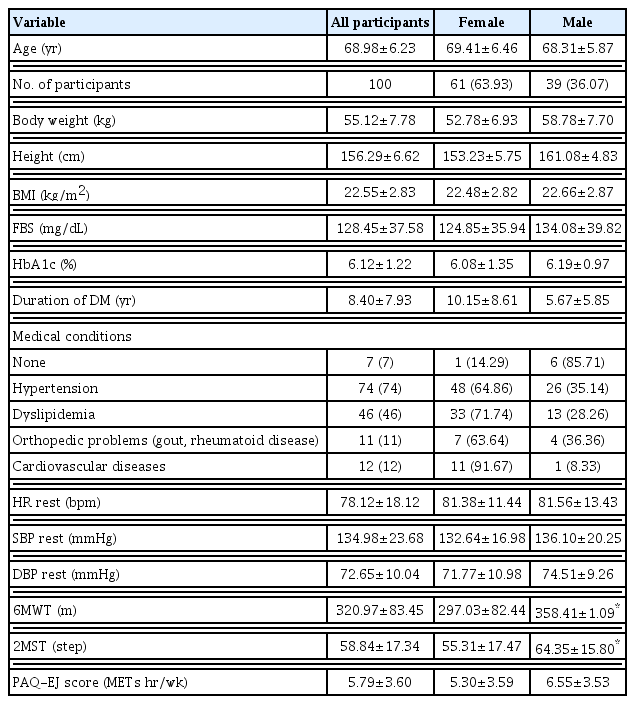
All participants in this study presented type 2 DM. General characteristics including age, gender, body weight, height, BMI, HR, SBP, and DBP are presented in Table 1. The period of diagnosis with type 2 DM averaged at roughly 8.40±7.93 years, and FBS were 128.45±37.58 mg/dL, and HbA1c 6.12%±1.22%, respectively. Most participants were diagnosed with other medical conditions, i.e., hypertension (75%), dyslipidemia (43%), orthopedic problems (rheumatoid disease) (11%), and cardiovascular disease (12%). Individuals exhibiting no comorbidities made up only 7% of all participants. The physical activity level was determined by using the Physical Activity Questionnaire for Elderly Japanese (PAQ-EJ), which is a self-administered physical activity questionnaire of older adults (Yasunaga et al., 2007). The PAQ-EJ score in female trend to lower than male (5.30±3.59 METs hr/wk vs. 6.55±3.53 METs hr/wk). The distance from the 6MWT and the number of steps from 2MST in female was significantly lower than male (6MWT: 297.03±82.44 m vs. 358.41±71.09 m, 2MST: 55.31±17.47 steps vs. 64.35±15.80 steps, respectively) (Table 1).
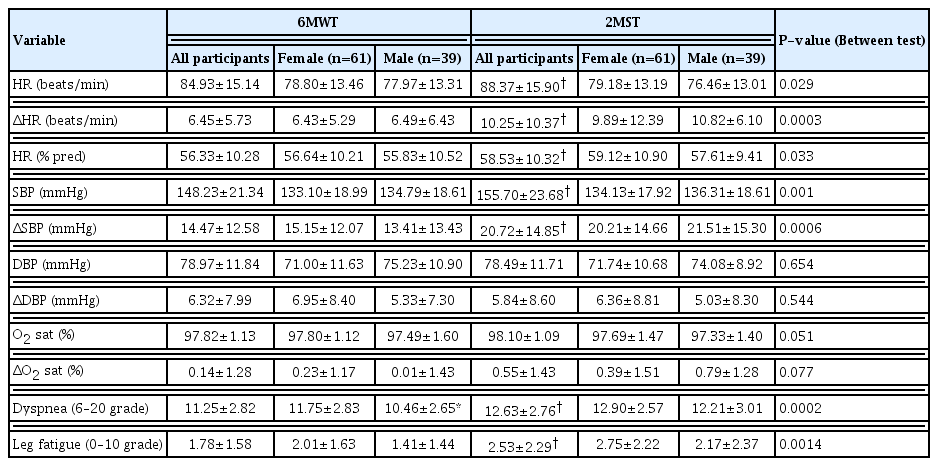
Comparative effects between 6MWT and 2MST on physiological changes, dyspnea, and leg fatigue in type 2 DM participants
To evaluate the cardiopulmonary endurance parameters, responses to the 6MWT and 2MST in female and male type 2 DM participants, this study measured hemodynamics, oxygen saturation, dyspnea score, and leg fatigue at baseline and immediately following the conclusion of both tests. Table 2 showed 2MST increasing of HR (84.93±15.14 beats/min vs. 88.37±15.90 beats/min, P=0.029), ΔHR (6.45±5.73 beats/min vs. 10.25±10.37 beats/min, P=0.0003), SBP (148.23±21.34 mmHg vs. 155.70± 23.68 mmHg, P=0.001), and ΔSBP (14.47±12.58 mmHg vs. 20.72±14.85 mmHg, P=0.0006) compared to 6MWT. The results of the 2MST were also significant in evaluating the degree of dyspnea (11.25±2.82 score vs. 12.63±2.76 score, P=0.0002) and leg fatigue (1.78±1.58 score vs. 2.53±2.29 score, P=0.0014) in type 2 DM compared with 6MWT (Table 2). These results suggest that the 2MST demonstrates a greater response amid physiological parameters, dyspnea, and leg fatigue than the 6MWT in type 2 DM participants. However, the dyspnea score in female was higher than male in the 6MWT (Table 2).
The correlation between 2-min step test and physical fitness tests in all DM participants
To explore the association of physical fitness tests, the distance from the 6MWT, the number of steps from 2MST, leg strength, and time from FTSST were measured in all type 2 DM participants. The data showed the number of steps in the 2MST was significantly positively correlated with distance in 6MWT (r=0.6995, P<0.0001) (Fig. 1A) and isometric leg strength (r=0.4292, P< 0.0001) (Fig. 1B). Moreover, the number of steps in the 2MST was significantly negatively correlated with the time of the FTSST (r=−0.405, P<0.0001) (Fig. 1C). These outcomes indicate that the 2MST—a cardiopulmonary endurance test employed in the elderly—predicted walking capacity, leg strength, and ability to change position from sitting to standing in patients with type 2 DM.
The correlation between 2-min step test, age, height, and body weight in all DM participants
The association between the 2MST, age, and height were observed in patients with DM (Fig. 2). The 2MST was weakly negatively correlated with age (r=−0.250, P=0.0123) (Fig. 2A) and barely positively correlated with height (r=0.205, P=0.04) (Fig. 2B). Nevertheless, the 2MST was not correlated with body weight in these participants (r=0.136, P=0.179) (Fig. 2C).
The optimal cutoff score, sensitivity, specificity, and AUC of the 2-min step test in all type 2 DM participants
To assess cardiorespiratory fitness prediction in patients with DM, the 2MST was analyzed via the ROC analysis. The results of this study showed that the number of steps amid the 2MST for optimal cutoff was ≤61 steps, with 92.24% sensitivity, 81.36% specificity, and AUC (95% confident interval) at 0.95 (0.91–0.99) (Table 3). The optimal cutoff score was also divided into female and male (female ≤59 and male ≤61 step, Table 3). This implied that patients with type 2 DM who performed the 2MST ≤61 steps were significantly associated with decreased cardiorespiratory fitness.
DISCUSSION
This study demonstrated that the number of steps in the 2MST was positively associated with the distance in the 6MWT, and leg strength. The 2MST was also negatively correlated with duration to perform the FTSST in type 2 DM patients. Moreover, our current study established that the optimal cutoff score of the 2MST was ≤61 steps to predict cardiorespiratory fitness in type 2 DM patients.
Maximal oxygen uptake is widely used as a key standard indicator for cardiorespiratory capacity or aerobic exercise capacity measurement. The 2MST and 6MWT are aerobic exercise capacity tests often used for evaluation of cardiorespiratory fitness in healthy or pathological populations. The 2MST was first introduced as part of the Senior Fitness Test by Rikli and Jones (1999a). So, participants were tested in the standing position and marched in place as fast as possible for 2 min while lifting the knees to a height midway between the patella and iliac crest. The 2MST has the advantage of requiring a short testing duration, limited space, and no expensive equipment. The 6MWT is a walking test whereby participants are instructed to walk along a flat corridor marked with a 30-m track pathway as quickly as possible, without running, for 6 min. Although the 6MWT is currently recommended for evaluating functional exercise capacity regardless of the setting, it requires minimal equipment, it is simple in its application and does not require practice - it is not practical in homes, medical offices, and communities due to its requirement of a hall 30 m long. The results of this study observed that the 2MST was able to induce cardiorespiratory stress-HR, SBP, dyspnea score, and leg fatigue, more so than the 6MWT. This indicates that shorter duration tests might be suitable as a reasonable estimate of cardiorespiratory capacity in participants. Whereas, the FTSST is used to assess functional lower extremity strength, transitional movements of sitting to standing, dynamic balance, and fall-risk in older adults (Whitney et al., 2005). Our data showed the number of steps in the 2MST was negatively correlated with the duration to perform FTSST, and positively correlated with leg strength. This suggested that lower extremity muscle strength performance is necessary to perform the step test. This result may imply that the 2MST test was a predictor of lower extremity muscle strength in patients with type 2 DM as well as the FTSST, and leg strength test.
A field test is commonly used to evaluate cardiopulmonary and musculoskeletal systems in clinical practice. It high clinical value amid the design exercise prescription for rehabilitation programs. The 2MST was employed to estimate the endurance exercise capacity, and as such it is practical and relevant for older, impaired, or pathological participants, especially those with comorbidities. Furthermore, our results presented a relationship between the decline of cardiorespiratory capacity, the reduction of leg strength, and loss of physical function in patients with type 2 DM. This study provides useful information on the 2MST to determine a person’s cardiorespiratory performance level, and thus identify the categorization of normal and poor cardiorespiratory fitness. Thus, the 2MST could be a field test option for the measurement of aerobic capacity, planning and progression of exercise protocols, as well as the prognosis of aerobic and physical capacity in type 2 DM.
Regarding previous studies reporting the validity and sensitivity of the 2MST as a predictor of aerobic capacity and exercise capacity. The result in elderly and healthy participants demonstrated that the number of steps performed during the 2MST was compared to the distances of the 6MWT in 60 participants for validity, r=0.935, and the sensitivity of the 2MST was high amid the number of steps achieved by both elderly and healthy participants (Chaturvedhi, 2021). The statistical validity, reproducibility, and sensitivity of the 2MST was also demonstrated in inpatients and outpatients who were participating in cardiopulmonary rehabilitation. Comparing the 2MST and 6MWT in 158 participants for validity where r=0.925, reproducibility revealed a minimal learning effect, and the sensitivity of the 2MST was high in all participating groups (Haas et al., 2017). Notwithstanding, there was no documentation employed as a cutoff score of 2MST to predict cardiorespiratory fitness in type 2 DM patients. Interestingly, our results first demonstrated the number of steps of 2MST ≤61 steps for optimal cutoff, with 92.24% sensitivity and 81.36% specificity.
There are some limitations concerning this study. First, as is already known, there are numerous factors such as sex, age, gender, weight, and height which could potentially affect physical fitness. This study has demonstrated that age and height held significant correlation with the number of steps in the 2MST. Moreover, the number of female participants outnumbered male participants. These factors might have influenced the number of steps despite the participants being encouraged throughout performance. Therefore, this study was analyzed the 2MST data by gender. Although the sample size is relatively small and the male participants were few, the tendency of the predictive values was quite acceptable. Hence, future studies should be studied at a larger size for each gender. Second, the presence of potential confounders such as medical conditions, medication use, and orthopedic problems, which might result in a bias, could not be avoided. Finally, although this study provided the optimal cutoff score of the 2MST to be an option of a field test for measurement of aerobic capacity with the flexibility to divide patients into normal and limited cardiorespiratory fitness, maximal oxygen consumption amid cardiopulmonary exercise testing is a gold standard to assess cardiorespiratory fitness levels.
In conclusion, our findings suggested that the number of steps in the 2MST showed positive correlation with the 6MWT distance, leg strength, and negative correlation with duration to perform the FTSST in type 2 DM patients. Lastly, this study established that the optimal cutoff score of the 2MST was ≤61 steps to predict cardiorespiratory fitness in type 2 DM patients.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
ACKNOWLEDGMENTS
This research project was financially supported by the Thailand Science Research and Innovation Fund, the University of Phayao (Grant No. FF65-UoE013), and the Exercise and Nutrition Innovation and Sciences Research Unit, Burapha University, Thailand. The authors also thank all participants for their generosity and willingness to participate in the study.