Effects of whole-body vibration combined with action observation on gross motor function, balance, and gait in children with spastic cerebral palsy: a preliminary study
Article information
Abstract
This study evaluated the effects of whole-body vibration (WBV) com-bined with action observation on gross motor function, balance, and gait in children with spastic cerebral palsy. The participants were randomized into the WBV combined with action observation (WBVAO) group (n=7) and the WBV group (n=7). The WBVAO group received WBV combined with action observation training, and the WBV group received WBV training for 4 weeks. Both groups received 30 min of training a day, 3 times a week. All participants completed the 5 times sit to stand (FTSTS) test, Timed Up and Go (TUG) test, pediatric reach test, 10-m walk test, 6-min walk test (6MWT), and timed up and down stair (TUDS) test before and after the training intervention. Moreover, the participant’s Gross Motor Function Measure (GMFM) and Pediatric Balance Scale (PBS) scores were assessed. Both the WBVAO and WBV groups demonstrated significant increases in the scores of FTSTS test, GMFM (D and E dimensions), PBS, TUG test, 6MWT, and TUDS test. The WBVAO group improved more significantly compared to the WBV group based on the scores of the FTSTS test, GMFM (D dimension), PBS, 6MWT, and TUDS test. WBV combined with action observation improved lower extremity functional strength, gross motor function, and balance and gait in children with cerebral palsy. These results suggest that WBV combined with action observation is both feasible and suitable for individuals with cerebral palsy.
INTRODUCTION
Cerebral palsy (CP) can be categorized according to the level of motor disturbance and the sites affected, with the spastic type being the most common (Himmelmann et al., 2005). It causes abnormal muscle tension including muscle weakness and spasms and impairments to balance and coordination, and for several children, it leads to difficulties in the achievement of gait and activities of daily living (Maruishi et al., 2001). To improve the Gross Motor Function Measure (GMFM) scores and balance and gait ability of children with CP, several intervention methods including progressive resistive exercise, treadmill gait training, and whole-body vibration (WBV) training have been evaluated (Han et al., 2019).
Among these training techniques, WBV training is considered to be a safe and effective method. WBV was recently introduced as a novel way to improve proprioceptive sense, bone density, balance, and motor skills (Ko et al., 2016). It is currently used as a clinical treatment to increase muscle strength and commonly involves performing a series of static or dynamic movements in a standing position on top of a vibration pad (Duquette et al., 2015). The vibrations produced stimulate the contracting muscle spindles and alpha motor neurons in accordance with the tonic vibration reflex. Stimulation of these reflexive muscle contractions alongside voluntary muscle contractions has been proposed as a method of improving function (Cardinale and Bosco, 2003). According to a systematic review by del Pozo-Cruz et al. (2012), the immediate effects of WBV include observed increases in oxygen consumption, muscle temperature, blood flow, and muscle power. WBV training consists of the user standing on the platform statically, or while performing dynamic movements for a fixed duration of time. Although WBV has gained such popularity, exact action of the therapy is yet to be determined (Nordlund and Thorstensson, 2007). This study provides WBV combined with action observation in children with spastic CP.
Motor learning is the ability to flexibly adapt to the environment when acquiring and performing motor techniques (Seidler, 2004). Motor learning combination with action observation to treat motor loss in the four limbs is proposed as a new treatment method for children with CP (Kim et al., 2014). Action observation is cognitively easier than the provision of verbal information only, and when patients carefully observe the detailed limb coordination used to perform an exercise, instinctive imitation may be provoked (Hecht et al., 2001). Previous studies provide contrasting opinions on action observation; however, these studies mostly focus on upper limb functional improvement and rehabilitation in children with CP. Studies examining gross motor function, balance, or gait are relatively insufficient. Therefore, this study aimed to examine the effects of WBV training and action observation in children with spastic CP.
MATERIALS AND METHODS
Children diagnosed with spastic CP and admitted at the National Transportation Rehabilitation Hospital, which is located in the Yangpyeong, Gyeonggi Province of Korea, participated in the study. Children with the following characteristics were included in the study: children aged 4–12 years who were diagnosed with spastic CP, children with no visual impairments, children who could respond to instructions provided by the researchers, and children with gross motor function categorized as levels 1–3 based on the Gross Motor Function Classification System Scale (GMFCS). Conversely, children with the following characteristics were excluded: children with scores >2 in the Modified Ashworth scale in their effected limb, children experiencing joint contracture, children who had experienced seizure within the past 6 months, or children with conditions that could not be controlled despite seizure medication. Finally, 14 participants were allocated randomly to the WBV combined with action observation (WBVAO) group (n=7) or the WBV group (n=7). This study protocol was approved by the Sahmyook University Institutional Review Board (2-1040781-AB-N-01-2016031HR), and the objective of the study and its requirements were explained to the participants. Written parental consent was provided for all of the participants; therefore, the rights of the human participants were protected.
Randomization and experimental procedures
Sixteen children who were receiving weekly or outpatient rehabilitation treatment from National Transportation Rehabilitation Hospital for their spastic CP were selected. Two of these 16 children were excluded from the study considering that their GMFCS scores were <3. To minimize any bias during selection, a stratified sampling method based on age and GMFCS stage was used. The number of children with CP who visited the hospital was small sample size and we could not make a control group without treatment for children with CP because that subjects needs an exercise therapy. Randomized sampling of each stratum was used to divide the participants into 2 groups of seven children: the WBVAO group and the WBV group. The WBVAO group completed WBV training along with action observation for 30 min a day, 3 days a week for a 4-week period, and the WBV group completed only the WBV training for 30 min a day, 3 days a week for a 4-week period. The experimental and control groups also performed 30 min a day of conservative physical therapy, 3 days a week for a 4-week period.
WBV combined with action observation training
WBV training along with action observation was performed to increase gross motor function, balance, and walking ability. The children assigned to the WBVAO group were instructed to maintain a standing posture on a vibration pad, supported and prevent falls by a back plate at the pelvis and spine. Children stood barefoot with feet parallel and knees in slight flexion (30°). The participants were instructed to watch a video on a 17-inch laptop screen from a distance of 50 cm during this time and were either instructed to follow or to not follow the actions demonstrated in the video. The model for the video comprised of actions performed by an average adult of normal body weight. It included six actions to improve lower extremity strength, balance, and gait (Liao et al., 2007). The participants were instructed to watch the different actions repeatedly throughout the experimental period. The participants were shown a video chosen by the physical therapist and instructed to repeat the action performed in the video, only proceeding to the next stage when they could perform the required action.
The first action was a standing position with feet parallel and the knees in slight flexion (30°). The second action comprised a sitting and standing movement over a limited range of motion, and the third action comprised a rotating movement from a standing position, training the ability to shift body weight from side to side. The fourth action involved shifting body weight forward and backward while standing in a split stance with the right foot forward, and the fifth action was similar as the fourth action except with the left foot forward. The sixth action was similar to the first one, with participants required to maintain a standing position with the knees in slight flexion (30°). Exercises for each of the six actions were performed after a minute of watching the video. Three minutes of physical training was completed for each action, followed by 1 min of rest. The total physical therapy time was therefore 30 min. The intensity of the WBV stimulation to improve muscle strength was 12–18 Hz, and it was applied by gradually increasing the intensity by 0.5 Hz starting with the intensity the each participant could withstand. The reason why the same intensity was not applied to all participants was because the age, disability, function, and sensory differences of CP were considered (Ruck et al., 2010). To increase the effects of the action observation, the therapy was conducted at a relatively quiet time of the day. The children were instructed to concentrate on the video for 1 min at a time, and the whole experiment was conducted by the same therapist. If the child complained of muscle fatigue or pain during the intervention, the therapy was terminated.
WBV training
The WBV group stood on the vibration pad in the same position and training protocols as the WBVAO group without action observation. During the 30 min of therapy, every 3 min of vibration training and 2 min of rest were repeated 6 times. The intensity of the WBV stimulation for muscular strength improvement was similar as the WBVAO group (12–18 Hz) and was applied by gradually increasing the intensity by 0.5 Hz starting from the intensity the participant could withstand.
Outcome measurements
Functional muscular strength measurement
The 5 times sit to stand (FTSTS) test was used to examine functional muscular strength of the lower extremity. The FTSTS test was initiated from a sitting position on a knee high bench with the hip joint in 90° flexion and the feet touching the floor. In this position, the lateral ankle bone was located 10 cm posterior to a perpendicular line drawn from the center of the knee. The time taken to perform the FTSTS test with the arms crossed and without any help from the upper extremity was recorded (Whitney et al., 2005). The interrater reliability for the FTSTS test defined using the intraclass correlation coefficient (ICC) was 0.95–0.99, with an ICC for test-retest reliability of 0.95–0.99 (Wang et al., 2012). To minimize measurement error, a research assistant who was independent of the child’s therapy performed three measurements before and after the experiment, and the average value was recorded.
Gross motor function measurement
The GMFM was used to assess gross motor function. The GMFM is divided into the following five domains: A (lying and rolling, 17 items), B (sitting, 20 items), C (quadruped and kneeling, 14 items), D (standing, 13 items), and E (walking, running, and jumping, 24 items) (Chang et al., 2017). This measure is used to provide overall standards for the participants’ gross motor function by evaluating their abilities rather than specific performance parameters. In this study, the results of the D (GMFM-D) and E (GMFM-E) factors were analyzed.
Balance function measurement
Balance function was evaluated using the Pediatric Balance Scale (PBS), Timed Up and Go (TUG) test, and pediatric reach test (PRT). The PBS comprises 14 tasks similar to activities of daily living. The items are scored on a 5-point scale, with zero denoting an inability to perform the activity without assistance and four denoting the ability to perform the task with complete independence. The maximum score is 56 points. The interrater reliability (ICC value) for the PBS test was 0.99, with an ICC value of 0.99 for the test-retest reliability (Franjoine et al., 2003). For the TUG test, participants were seated in a chair with armrests and subsequently instructed to stand (using the armrests, if desired) and walk as quickly and safely as possible for a distance of 3 m. The participants subsequently turned around, returned to the chair, and sat down. The time from the point at which their spine left the back of the chair until they returned to that same position was recorded using a stopwatch (Williams et al., 2005). TUG was measured 3 times and the average was used for analysis. The PRT is a dynamic balance test. Participants were instructed to stand 10 cm from the wall so that their shoulders were perpendicular to the reach measurement device. Participants extended their arm horizontally and placed a closed first against the sliding handle. Values for the ICC for test-retest and intertester reliability for children with CP ranged from 0.54 to 0.88 and 0.50 to 0.93, respectively (Bartlett and Birmingham, 2003). PRT was measured 3 times and the average was used for analysis.
Gait function measurement
Gait function was examined using the 10-m walk test (10MWT), 6-min walk test (6MWT), and timed up and down stair (TUDS) test. Gait velocity was measured using the 10MWT. Participants completed three trials in succession, with a brief seated or standing rest as needed between trials. An ICC of 0.81 for the 10MWT has been reported across participants (Thompson et al., 2008). The 6MWT is a self-paced walking capacity test at a fast speed. Participants were instructed to walk on an indoor straight course for 6 min and were permitted to slow down, stop, and rest as necessary (Brehm et al., 2017). The TUDS test was used to assess functional walking ability related to daily life. Before the starting signal for the TUDS test, the participants were instructed to “climb the stairs up and down as fast as possible without falling down.” The participants waited for the starting signal with both feet on the ground, and timing commenced after the starting signal. The participants subsequently went up and down a flight of 10 stairs, and when both feet reached the ground, the time recording ended. The participant could rest on the way up or down; however, the time was continuously recorded. If required, handrails could be used during the test (Zaino et al., 2004). To minimize measurement error, 10MWT, 6MWT, and TUDS were performed by a research assistant who was blinded to the child’s therapy before and after the experiment, and the average value was recorded.
Data analyses
All statistical analyses were performed using the IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Descriptive statistics for the baseline variables were calculated to characterize and compare the two study groups. The Shapiro–Wilk test was used to determine whether the general characteristics and the outcome measures of the participants were normally distributed. Means and standard deviations are reported for the normally distributed variables. Independent t-tests were used to analyze changes in the dependent variables between groups. Paired t-tests were performed to compare the dependent variables pre- and postintervention within each group (intragroup). A P-value <0.05 was considered significant.
RESULTS
The characteristics of the 14 participants who completed the experiment are shown in Table 1. No differences in age, height, weight, sex, dominant arm, or GMFCS score were detected between the two groups at baseline.
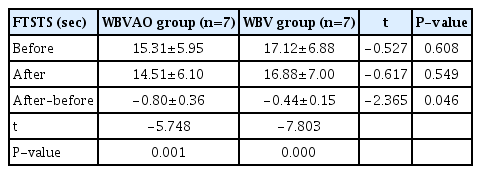
Functional muscular strength measurement
Differences in lower extremity functional strength after the intervention are shown in Table 2. Both groups showed significant differences in the FTSTS test scores (WBVAO group, P=0.001; WBV group, P=0.000). There were significant differences between the two groups postintervention (P=0.046).
Gross motor function measurement
A comparison of GMFM within and between groups is shown in Table 3. The WBVAO group showed significant differences in the GMFM-D (P=0.000) and GMFM-E (P=0.002) factors. The WBV group showed significant differences postintervention in the GMFM-D (P=0.004) and GMFM-E (P=0.002) factors. There were significant differences in the GMFM-D factors between the two groups postintervention (P=0.037).
Balance function measurement
Comparisons of the balance functions within and between groups are shown in Table 4. The WBVAO group showed significant differences in the PBS (P=0.000), TUG test (P=0.002), and PRT (P=0.047) scores. The WBV group showed significant differences in the PBS (P=0.000) and TUG test (P=0.007) scores. There were significant differences in the PBS scores between the two groups postintervention (P=0.028).
Gait function measurement
Comparisons of the gait functions within and between groups are shown in Table 5. The WBVAO group showed significant differences in 10MWT (P=0.003), 6MWT (P=0.000), and TUDS test (P=0.000) scores. The WBV group showed significant differences in 6MWT (P=0.001) and TUDS test (P=0.001) scores. There were significant differences in 6MWT (P=0.024) and TUDS (P=0.012) scores between the two groups.
DISCUSSION
In a child with CP, muscle weakness is one of the factors that decreases motor functions, and these decreases in motor function even affect the control of body functions (Damiano and Abel, 1996). Dodd et al. (2003) reported the results of muscle strengthening exercises for the lower extremity in children with spastic paraplegia. Improvements in lower extremity muscular strength and the D and E factors of the GMFM scale were found (P<0.05). In this study, the GMFM-D factor for the WBVAO group showed improvement from 79.53% in the pretest to 83.87% in the posttest, and the GMFM-E factor showed improvement from 68.64% to 71.22% in the pre- and posttests, respectively. The WBV control group showed an increase from 77.65% to 80.21% for the GMFM-D factor and an increase from 63.87% to 66.05% for the GMFM-E factor in the pre- and posttest, respectively. Both of these increases were significant (P<0.05). Moreover, in the comparison between groups, the GMFM-D factor showed significant differences in both the pre- and posttest results (P<0.05). These GMFM results can be interpreted as an increase in the participant’s mobility and the ability to perform activities of daily living (Dickin et al., 2012).
Tupimai et al. (2016) confirmed that WBV training stimulates proprioceptive sensations through the soles of the feet, reflexively causing muscle contractions that increase knee extensor muscle strength, and kinetic postural ability in a standing posture. Action observation accompanies a direct multisensory effect, helping the patient to clearly visualize the exact positioning for each exercise. This was supported by the results of the WBVAO group in this study since a more significant change in the GMFM results was observed compared to the WBV group. Although conducted in a relatively short amount of time, the repeated viewing of the videos (including shifting the body weight forward and backward), along with the sitting and standing training, allowed for an easier understanding of the specific positions for each action and their order. This increased the exercise learning effects.
Balance comprises stability in both static (including standing or sitting) and dynamic (including reaching with the hands or walking) postures. According to these definitions, children with CP lack the voluntary postural stability required for daily activities. The body’s reactive balance ability in response to external change is also affected due to severe loss of muscular strength, abnormal muscle tension, and a lack of motor control (Saether et al., 2013). In this study, the PBS score of the WBVAO group increased significantly from 43.71 in the pretest to 45.71 in the posttest (P<0.05). The WBV group also showed a significant increase in the PBS score from 40.42 in the pretest to 41.71 in the posttest (P<0.05). Furthermore, a significant difference in both the pre- and posttest results between the groups was observed (P<0.05). These PBS results can be interpreted as an increase in dynamic balance ability. This study induced symmetrical weight bearing and functional lower extremity muscular strengthening by stimulating proprioceptive sensibility through WBV training in a standing position (Gandevia, 2001). Additionally, voluntary body weight movement with the use of action observation and posture regulation training on top of the vibration pad led to an increase in dynamic stability and lower extremity regulation ability. This may be due to the strengthening of muscle activity in the hip, knee, and ankle joint. Therefore, certainly, PBS factors, including looking over the left or right shoulder while standing or alternately putting each foot on top of a pad without holding onto anything, were significantly more improved in the WBVAO group compared to the WBV group.
Kumban et al. (2013) conducted specific training on sitting and standing with 21 children with CP aged 6–15 years. The PRT distances increased from 24 cm pretraining to 28.25 cm posttraining. In the current study, the PRT score was significantly higher in the posttest 13 cm compared to the pretest 12.28 cm in the WBVAO group (P<0.05). The PRT score for the WBV group also increased from 11.21 cm in the pretest to 11.64 cm in the posttest. The PRT results indicate an increase in postural stability in the standing position and in dynamic balance ability. It could be theorized that these differences result from the action observation training stimulating the excitability of the primary motor cortex. Visualization may affect the cognitive areas associated with constructing motor memory through imitation and the parts associated with understanding actions through observation (Gangitano et al., 2001).
A child with CP presents with symptoms including muscular strength weakness due to a damaged central nervous system, abnormal muscle tone including spasticity, a decrease in sensory function, a loss of the abilities to regulate muscle, and decreased balance ability due to an unstable posture. As a result, these children experience difficulties in achieving independent walking and activities of daily life (Maruishi et al., 2001). Due to these reasons, improved walking ability, including gait speed, gait stamina, and stair walking become important treatment goals for children with CP.
In this study, the WBVAO group showed a significant improvement in 10MWT score with the time taken to complete the test decreasing from 13.60 sec in the pretest to 13.10 sec in the posttest (P<0.05). In the WBV group, the 10MWT time decreased from 13.71 sec in the pretest to 13.47 sec in the posttest. There was no significant difference between the groups in the pre to posttest changes. These improvements in 10MWT times signify an improvement in gait speed. Hsu et al. (2003) reported a close association between gait speed and the muscular strength of the ankle plantar flexors, knee extensors, and flexors and extensors of the hip joint. In this study, the action observation performed by the WBVAO group along with the WBV training stimulated proprioceptive sensibility, increased the muscular strength of the knee extensors, and heightened the understanding of actions including gait using different directions of weight shift in a standing position. Despite the short training period, these effects may have contributed to the significant difference in the 10MWT results between the WBVAO and WBV groups. Meyer-Heim et al. (2009) examined gait endurance in 22 children with spastic CP aged 4–12 years following 5 weeks of robot-assisted gait training. Gait endurance improved from 176.3 m before training to 199.5 m after training. In the current study, the WBVAO group’s 6MWT distance significantly increased from 284.28 m in the pretest to 300.71 m in the posttest training (P<0.05). The 6MWT distance also significantly increased from 269.28 m in the pretest to 280 m in the posttest for the WBV group (P<0.05). Moreover, there was a significant difference in the pre–post training changes (P<0.05). Wilkinson et al. (2008) stated that muscular strength training of the lower extremity is crucial for improving gait endurance. This study has the following advantage: the comparison between the WBV training group versus the WBVAO group was observed in this study. This allowed the examination of functional muscle strengthening due to the stimulation of the proprioceptive receptors while standing on the vibration pad and the investigation of the difference between the observed models and the participant’s internal plans (Petrosini et al., 2003). This is supported by previous research stating that treatments using timed feedback supports symmetrical recording (Winstein et al., 1989).
Tarakci et al. (2016) investigated the effects of 12 weeks of balance training using Nintendo’s Wii-fit’s balance-based video games in 30 children aged 5–18 years. The time taken to complete the 10-step stair climbing test significantly decreased from 10.32-sec pretraining to 8.42-sec posttraining (P<0.05). In this study, the TUDS test scores improved significantly in the WBVAO group, with a decrease in the time taken from 22.95 s in the pretest to 21.98 sec in the posttest (P<0.05). Similarly, the TUDS scores for the WBV group also improved significantly, with a decrease in time from 25.35 sec to 24.78 sec in the pre- and posttest, respectively (P<0.05). A significant pre–post time difference between the two groups was also observed (P<0.05). This improvement in the TUDS test indicates an increase in functional gait ability in daily life. You et al. (2005) stated that there is a direct relationship between forwards, backwards, left, and right lower extremity weight shift movements and symmetrical weight bearing ability in a standing position, and also functional gait ability. Lay et al. (2006) stated that strengthening the knee extensors, decreases the likelihood of postural perturbation occurring during stair walking. In the current study, it can be hypothesized that a significant difference between the WBV group and the WBVAO group was observed due to an increase in muscular activity resulting from symmetrical weight bearing during WBV training and its stimulation of proprioceptive sensibility. Improvement in stair climbing, which is a functional gait activity, is possibly due to the voluntary forward, backward, left, and right weight shift movements of the lower extremity during the action observation.
This study has the following limitations: this study has a short 4-week intervention period; the frequency of application in WBV is limited in this study; prior studies, which may serve as reference studies, are not available; and this study comprises a small sample size. This makes it difficult to generalize the findings to all children with CP. It is also difficult to control all the factors that might affect the child’s activities of daily living. Furthermore, several of the participants had a short attention span while concentrating on the action observation, making it difficult for the treatment to last long as planned. Some of the CP in the WBVAO group did not follow the actions demonstrated in the video because of severity. This could be explained by the fact that children with spastic CP are not only impaired by the regulation ability of the muscular system and sensory deprivation but are also deprive of cognitive function (Chan and Miller, 2014).
ACKNOWLEDGMENTS
This study was supported by a grant from the NRF (NRF-2018R1D1A1B07045746), which is funded by the Korean government.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.